Abstract
A core feature of human drug dependency is persistence in seeking and using drugs at the expense of other life goals. It has been hypothesized that addiction is associated with overvaluation of drug-related rewards and undervaluation of natural, nondrug-related rewards. Humans additionally tend to persist in using drugs despite adverse consequences. This suggests that the processing of both rewarding and aversive information may be abnormal in addictions. We used fMRI to examine neural responses to reward and loss events in opiate-dependent patients receiving methadone maintenance treatment (MMT, n=30) and healthy controls (n=23) using nondrug-related stimuli. Half of the patients were scanned after/before daily methadone intake (ADM/BDM patient groups). During reward trials, patients as a whole exhibited decreased neural discrimination between rewarding and nonrewarding outcomes in the dorsal caudate. Patients also showed reduced neural discrimination in the ventral striatum with regard to aversive and nonaversive outcomes and failed to encode successful loss avoidance as a reward signal in the ventral striatum. Patients also showed decreased insula activation during the anticipation/decision phase of loss events. ADM patients exhibited increased loss signals in the midbrain/parahippocampal gyrus, possibly related to a disinhibition of dopamine neurons. This study suggests that patients with opiate dependency on MMT exhibit abnormal brain activations to nondrug-related rewarding and loss events. Our findings add support to proposals that treatments for opiate addiction should aim to increase the reward value of nondrug-related rewarding events and highlight the importance of potential abnormalities in aversive information processing.
Similar content being viewed by others
INTRODUCTION
Drug addiction is a major problem worldwide, contributing significantly to the global burden of disease. A core manifestation of human addiction is a focus on seeking and using drugs, to the neglect of nondrug-related activities (Hyman et al, 2006). This has led to a hypothesis that human drug addictions are associated with overvaluation of drug-related rewards and undervaluation of ‘natural’, nondrug-related rewards (Diekhof et al, 2008; Hyman et al, 2006). Drug use often continues despite repeated aversive consequences, such as the need to engage in criminal activity and failure to maintain social roles (Hyman et al, 2006). This suggests that in human drug addiction not only the processing of positive (reward) information but also the processing of negative (aversive) information is abnormal.
It has been hypothesized that drugs of dependence ‘hijack’ brain systems for learning about rewards and punishments, such that drug-related stimuli become overvalued and nondrug-related stimuli become undervalued (Koob and Volkow, 2010). Brain regions proposed to be affected include the mesolimbic dopamine system, given that most drugs of addiction exert actions on this system, and dopamine is critical for processing information about reinforcing stimuli (Berridge, 2007; Hyman et al, 2006). Phasic dopamine encodes an error in the prediction of rewards (Schultz, 1998), serving as a ‘teaching’ signal in the brain mediating the learning of associations (Montague et al, 1996) and/or the attribution of ‘incentive salience’ to reward-related stimuli (Berridge, 2007). Addictive drugs have a common action of triggering increases in dopamine in limbic regions (Hyman et al, 2006). Drug-induced firing of dopamine is believed to facilitate the attribution of incentive salience to drugs and drug-associated cues (Volkow et al, 2009). If drug use becomes chronic, repeatedly perturbing the dopamine system, neuroadaptive long-term changes may be triggered in dopaminergic and other pathways (Volkow et al, 2009). Consistent with this, a number of studies have reported a reduction in dopamine D2 receptors and a reduction in dopamine release in the striatum of drug-dependent humans, which can persist for months after detoxification. This has been reported for a variety of addictive drugs, including cocaine, alcohol, methamphetamine, and nicotine (Fehr et al, 2008; Volkow et al, 2009; Wang et al, 1997). These persistent neuroadaptive changes may result in reduced sensitivity to reinforcers (Koob and Volkow, 2010).
Most neuroimaging studies of human addiction have focused on examining neural responses to drug-related cues. These studies have typically reported that drug-related cues trigger activations in brain regions such as the striatum and medial prefrontal cortex, which normally activate in response to nondrug-related rewards in healthy subjects (Diekhof et al, 2008; Heinz et al, 2004; Sell et al, 2000; Wrase et al, 2006). Fewer studies have investigated neural responses to nondrug-related rewards in dependent individuals. Decreased neural responses to nondrug-related rewards have been reported with cocaine (Garavan et al, 2000; Goldstein et al, 2007), alcohol (Wrase et al, 2007), nicotine, (Buhler et al, 2010; Peters et al, 2011) and opiate (Martin-Soelch et al, 2001) misuse. Investigation of neural responses to aversive stimuli in addiction is rare. Only one study, to our knowledge, has reported reduced ventral striatal activation during anticipation of loss in detoxified alcohol dependency (Wrase et al, 2006).
Here we used fMRI to investigate neural responses to both rewarding and aversive, nondrug-related stimuli, in a clinically stable population of opiate-dependent patients receiving methadone maintenance treatment (MMT). We hypothesized that patients would exhibit abnormalities in processing rewarding and loss events, in regions such as the striatum, midbrain, amygdala-hippocampal complex, insula, and medial prefrontal cortex, which have been associated with processing reinforcer information (Liu et al, 2011). In addition, we investigated whether neural responses in patients would differ depending on whether patients were scanned before or after their daily methadone dose (Langleben et al, 2008).
MATERIALS AND METHODS
Participants
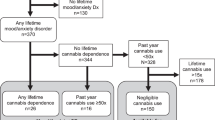
The study was approved by the Tayside Committee administered by the East of Scotland Research Ethics Service, and written informed consent was obtained from all participants. Data were acquired from a group of thirty-five patients with a diagnosis of DSM-IV opiate dependence receiving MMT and a group of twenty-six healthy controls. All patients were recruited from the NHS Fife Addiction Service, United Kingdom, with a history of poly-substance drug misuse and heroin as the main ‘drug of choice’ preceding MMT.
The inclusion criterion for MMT patients was more than 3 years of regular and daily heroin consumption, followed by more than 6 weeks at a stable dose on a MMT prescription program. Exclusion criteria for all participants were any neurological disorder, claustrophobia, other DSM-IV diagnosis or evidence for current illicit drug misuse. Comorbidity was assessed using the Mini International Neuropsychiatric Interview (MINI Plus V. 5.0). Just before scanning, all participants were screened using urine toxicology to test for illicit drug use. One patient tested positive for opiates other than methadone and so was excluded from the analysis. Seven other participants were excluded from the analysis because of inability to tolerate the scanner environment (two patients), difficulties remaining awake in the scanner (three controls and one patient), and not understanding the task properly (one patient).
Demographic details of subjects included in the analysis (23 controls; 30 patients) are presented in Supplementary Table S1. Patients and controls were matched on the basis of gender (all males) and age (range: 20–40 years; t(33.9)=−1.6, p=0.11). Controls had higher estimated pre-morbid IQ (t(51)=2.67, p=0.01) according to the National Adult Reading Test (NART) (Nelson and Wilson, 1991) and current IQ measured using the Wechsler Abbreviated Scale of Intelligence (WASI), vocabulary and matrix reasoning subtests (t(50)=3.32, p=0.002).
Symptoms of depression and anxiety were assessed before scanning using the Hospital Anxiety and Depression Scale (HADS) (Zigmond and Snaith, 1983). As is typical with alcohol and other types of dependency, patients had higher depression symptom scores than healthy controls (t(50.9)=−3.17, p=0.003) with a trend for higher anxiety scores (t(50.9)=−1.92, p=0.061). However, none met DSM-IV criteria for major depressive disorder at the time of the scan. Fifteen of the twenty-three controls and twenty-nine of the thirty patients were tobacco smokers with patients having a higher Fagerstrom Test score for nicotine dependence (Heatherton et al, 1991) (t(51)=−3.73, p<0.001). Smokers were not in a withdrawal state at the time of scanning. Differences between the patient and control groups (IQ, depression, anxiety, and nicotine dependence) were accounted for in the analysis (Supplementary Information).
Half of the MMT patients were scanned 90 min after daily methadone (ADM), with the others (BDM) scanned just before daily methadone. Ninety minutes was chosen to take account of the pharmacokinetics of methadone oral administration, aiming for a maximum ADM group methadone plasma concentration (Dyer and White, 1997; Langleben et al, 2008). Patients were randomly allocated to the ADM and BDM groups. As the scanning schedule time was fixed, to avoid possible withdrawal issues, patients were asked to adjust (4–5 days before scanning) their daily time of taking methadone so that they did not have to wait to take their methadone at the time of scanning, regardless of which group they were assigned to. The ADM and BDM groups did not differ in daily methadone dose, age, NART, WASI, HADS-Depression, or HADS-anxiety scores (all p>0.14). The half-life of methadone is 24–48 h in long-term opioid users, and a once daily dose of methadone is believed to induce a steady state (Curran et al, 2001). All patients were established on daily methadone administration. Symptoms of early withdrawal include agitation, anxiety, muscle aches, and sweating. No patients experienced these symptoms.
Paradigm
During scanning, participants performed a reward and loss learning task (Figure 1a). In this task, there were three types of trial: reward, neutral, and loss. Each type of trial was associated with one of three pairs of fractal pictures (roughly shaped as squares, circles, and triangles). Associations with different picture pairs were randomized across subjects.
Experimental task and behavioral results. (a) Experimental task. On each trial, participants select one of two fractal pictures, subsequently, and outcome is displayed. On reward trials, one of the pictures is associated with a 0.7/0.3 probability of delivering ‘win’/‘nothing’, whereas the other picture has complementary probabilities. Similarly, on the loss trials, one of the pictures leads to ‘nothing’/‘loss’ with probabilities 0.7/0.3, whereas the other picture has complementary probabilities. A neutral condition leads to outcomes ‘no-change’/‘nothing’ with probabilities as in the reward and loss trials. t1, duration of the first screen. (b) Behavioral Choice. Proportion (percentage) of the number of times that participants selected the high-rewarding stimulus on reward trials, the high loss avoidance stimulus on the loss trials, and the stimulus more associated with the ‘No-Change’ image on the neutral trials. (c) Reaction time in seconds. Error bars denote SEM.
At the beginning of each trial, a fractal pair was presented (each fractal randomly assigned to the left or right of the screen), and the volunteer had to select one of the pictures via a button press. Once a fractal picture had been selected, it appeared circled in red, and then an outcome was displayed. On each of the reward, neutral, and loss trials, the possible outcomes were win-one-point/nothing, no-change-in-points/nothing, and lose-one-point/nothing, respectively. On reward trials, a given fractal stimulus (high-reward probability stimulus) had a fixed probability 0.7/0.3 of delivering win/nothing, whereas the other fractal stimulus (low-reward probability stimulus) had complementary probabilities. Similarly, on the loss trials, one of the pictures (high loss avoidance probability stimulus) had fixed probabilities 0.7/0.3 of delivering nothing/loss and the other picture (low loss avoidance probability stimulus) had complementary probabilities.
Participants agreed to accumulate as many points as possible and were told that, at the end of the scanning session, wins and losses would be summed, and they would receive a gift voucher for an amount based on their net points. Participants were told they could exchange the gift voucher for a variety of items in shops such as books, music, or clothes. A gift voucher was chosen instead of money, as we wished to use a nondrug-related reinforcer, and money could have been associated with drugs (Diekhof et al, 2008) (see Supplementary Information for further details on the task).
Behavioral Analyses
A mixed ANOVA was used to assess the effects of valence (reward, neutral, and loss) and group (controls, patients) on the number of high-probability stimuli selected and reaction times.
fMRI Analyses
fMRI images were acquired using a 3T Siemens Magnetom Tim Trio MRI scanner. SPM8 (http://www.fil.ion.ucl.ac.uk/spm) was used for preprocessing (Supplementary Information) and analyses.
For the first level analysis, an event-related design was implemented with the picture pair onset time (anticipation/decision time) and the outcome time modeled as truncated delta functions. A general linear model was implemented with events for each trial type onset (reward, neutral, and loss) and the six outcomes (two reward outcomes win/no-win, two neutral outcomes, and two loss outcomes loss avoidance/loss), each considered as a separate regressor. The six head motion realignment parameter estimates were included as covariates of no interest. Regressors of interest were convolved with the SPM8 hemodynamic response function without time or dispersion derivatives.
To examine neural activity at the anticipation/decision time, we computed the reward vs neutral and loss vs neutral contrasts. To examine neural activity at the outcome time, win vs no-win and the loss avoidance vs loss contrasts were calculated. Contrast images for each subject were taken to the second level of random effect analyses, to test for within group activations (one-sample t-tests) and between groups (controls vs patients) differences (two-sample t-tests). An additional second level analysis compared activations between the two patient groups (ADM vs BDM) with a two-sample t-test.
During reward learning tasks, activity in the ventral striatum is thought to be better described by reward prediction errors (mismatch between the predicted and actual outcome) rather than by a simple reward vs no-reward contrast (Niv et al, 2012). To further examine activity in the ventral striatum, we used a standard reinforcement learning algorithm that estimated prediction errors for the reward and loss trials at the outcome time of the task. Prediction errors generated by the model were used to investigate the encoding of prediction errors in the ventral striatum (Supplementary Information).
We investigated whether brain abnormalities observed in the MMT patient group correlated with the daily methadone dose. This analysis was limited to a priori regions of interest that usually activate during the processing of rewarding and aversive information—the striatum, midbrain, amygdala-hippocampal complex, insula, and medial prefrontal cortex (Liu et al, 2011)—and that exhibited abnormalities on between group comparisons. The dependent variable in this analysis was the mean value of the parameter estimates across voxels within a 10 mm diameter sphere, centered at the maximum peak coordinates of the regions that showed between group differences.
Unless otherwise stated, all analyses regions are reported as significant at a whole brain p<0.05 cluster level. This was achieved by a simultaneous requirement for a voxel threshold of p<0.005 and a minimum cluster size of 68 continuous voxels, these parameters being identified using Monte Carlo simulations (Slotnick et al, 2003).
RESULTS
Behavioral Analyses
Both MMT patients and controls learned to select most often the high-rewarding stimulus on the reward trials and the high loss avoidance stimulus on the loss trials (p<0.001 for both valences and both groups) (Figure 1b, Supplementary Table S2). The mixed ANOVA for behavioral choice showed a significant effect of valence (F(1.7,87)=6.4, p=0.004) and no significant effect of the group (controls vs patients) or the group by valence interaction. Post hoc Bonferroni corrections showed that participants chose the high-probability stimulus more frequently on the reward trials than on the neutral (p=0.012) and loss trials (p=0.001).
The mixed ANOVA for reaction times showed a significant effect of valence (F(2,102)=53.5, p<0.001) with longer reaction times for the loss condition compared with the reward and neutral conditions (Figure 1c). Slower reaction times for loss event decision making have been reported in a similar task (Pessiglione et al, 2006). As discussed by the authors, this likely indicates physiological differences between selecting an action that leads to a reward and avoiding an action that leads to a loss. A significant effect of the experimental group was present (F(1,51)=5.41, p=0.024) with patients being slower. There was also a significant valence by group interaction (F(2,102)=3.43, p=0.036), with controls showing a trend for faster reaction times on neutral compared with reward trials, while patients did not show this pattern.
To compare choices and reaction times between the two patient groups, the same analyses were repeated with the factors valence and group (ADM, BDM). There was no significant effect of group or group by valence interaction on behavioral choice or reaction time, indicating a similar performance from both groups of patients.
We tested for differences across groups (controls vs patients and ADM vs BDM) in the reinforcement learning model parameters  (learning rate) and
(learning rate) and  (inverse temperature), and no significant differences were observed (Supplementary Information).
(inverse temperature), and no significant differences were observed (Supplementary Information).
Neuroimaging Analyses: Rewards
On reward trials, for the contrast win>no-win at the outcome time, controls activated a network of brain regions usually reported as active during rewarding events, such as the ventral and dorsal striatum, midbrain, medial prefrontal cortex and amygdala–hippocampal complex (Figure 2a). MMT patients also exhibited activations in the ventral striatum, medial prefrontal cortex and amygdala–hippocampal complex (Figure 2b).
Neural responses during reward trials for the contrast win>no-win at the outcome time of the task. Brain regions active in controls (a) and in patients (b) during reward trials for the contrast win>no-win. (c) Controls exhibited greater activation than patients for the contrast win>no-win in the dorsal caudate (d) Mean value of parameter estimates across voxels within a 10 mm diameter sphere, centered at peak coordinates (−20, 22, 12) of the left dorsal caudate region where patients differed significantly from controls. ADM/BDM, patients scanned after/before the daily methadone intake; DC, dorsal caudate; mPFC, medial prefrontal cortex; S, striatum; VS, ventral striatum. Regions significant at p<0.05 whole brain corrected as described in the methods, overlay on an average structural scan. Error bars denote SEM.
Significant between-group differences (patients vs controls) were found bilaterally in the dorsal caudate (Figure 2c, Supplementary Table S3) ((−20, 22, 12), t=4.06; (16, 26, 4), t=3.22). These between-group differences were driven by abnormalities in the MMT patient group, with patient’s neural responses in the dorsal striatum discriminating less between obtaining a reward and nothing (Figure 2d). A comparison for the contrast win>no-win between the two patient groups (ADM vs BDM) did not identify significant differences in the caudate (Supplementary Table S4). This indicates that caudate abnormalities contrasting patients (as a whole) and controls were not due to methadone having been recently taken or not.
Both controls and patients exhibited significant encoding of reward prediction errors in the ventral striatum (Supplementary Figure S1) with no significant differences between groups.
At the anticipation/decision time of the task (trial onset), for the contrast reward>neutral, both controls and MMT patients activated the ventral striatum, insula and dorsomedial prefrontal cortex. No significant differences between patients and controls, or between the two patient subgroups, were found in regions of interest (Supplementary Figure S2, Supplementary Tables S5 and S6).
Neuroimaging Analyses: Losses
On loss trials, at the outcome time, controls activated the ventral striatum for the contrast loss avoidance>loss. This is consistent with previous findings (Pessiglione et al, 2006), indicating that in the case of the ventral striatum avoiding a loss resulted in similar neural activity to obtaining a reward (Figure 3a, Supplementary Table S7).
Neural responses during loss trials for the contrast loss avoidance>loss at the outcome time of the task. (a) Controls activated the bilateral ventral striatum for the contrast loss avoidance>loss. (b) In contrast, patients failed to show this activation. (c) Controls exhibited stronger activation than patients for the contrast loss avoidance>loss in the bilateral ventral striatum. (d) Mean value of parameter estimates across voxels within a 10 mm diameter sphere, centered at peak coordinates (−14, 6, −10)/(16, 6, −10) of the left/right ventral striatal regions where patients differed significantly from controls. ADM/BDM, patients scanned after/before the daily methadone intake; VS, ventral striatum. Regions significant at p<0.05 whole brain corrected. Error bars denote SEM.
Notably, MMT patients failed to show activation in the ventral striatum for discriminating loss avoidance>loss (Figure 3b). This resulted in significant between-group differences in the bilateral ventral striatum for the contrast loss avoidance>loss (Figure 3c and d, Supplementary Table S9) ((−14, 6, −10), t=4.64; (16, 6, −10), t=3.79). Significant differences between patients and controls were also found in the ventral striatum when considering the encoding of loss avoidance prediction errors (Supplementary Figure S3). When comparing the two patient subgroups (ADM, BDM), either using the contrast loss avoidance>loss or the loss avoidance prediction error signal, there were no significant differences in activity in the ventral striatum (Supplementary Table S10). This again suggests that altered ventral striatal responses in patients were not driven by just having taken methadone.
Considering the opposite contrast, loss>loss avoidance at the outcome time, both controls and MMT patients activated the dorsal anterior cingulate and other regions (Figure 4a and b, Supplementary Table S8). Patients exhibited a cluster of activation that extended throughout parts of the midbrain and into the parahippocampal gyrus (Figure 4b). This resulted in a significant between-group difference, with patients demonstrating stronger neural responses to loss>loss avoidance (in the midbrain/parahippocampal gyrus) than controls (Figure 4c and d, Supplementary Table S9) ((−18, −18, −20), t=3.73; (16, −18, −20), t=3.93). The between-group comparison (ADM vs BDM) showed that the activation in the midbrain/parahippocampal gyrus was stronger for patients who were scanned after taking methadone (Figure 4d, Supplementary Table S10). Taking the MMT patients as a whole, the neural response for the contrast loss>loss avoidance in the left midbrain/parahippocampal gyrus correlated positively with daily methadone dose (r(30)=0.47, p=0.009) (Figure 4e). This indicates that stronger midbrain/parahippocampal gyrus activation during loss vs loss avoidance was associated with increased methadone dose.
Neural responses during loss trials for the contrast loss>loss avoidance at the outcome time of the task. (a) Controls activated regions such as the posterior midbrain and the dorsal anterior cingulate for the contrast loss>loss avoidance. (b) Patients displayed a cluster of activation that extended through the midbrain and parahippocampal gyrus for the contras loss>loss avoidance. (c) Patients exhibited stronger activation than controls in the midbrain/parahippocampal gyrus for the contrast loss>loss avoidance. (d) Mean value of parameter estimates across voxels within a 10 mm diameter sphere, centered at peak coordinates (−18,−18, −20)/(16, −18, −20) of the left/right midbrain-parahippocampal gyrus regions where patients differed significantly from controls. (e) Correlation with the methadone daily dose in milligrams for the left midbrain-parahippocampal gyrus of patients. The dependent variable is the mean value of parameter estimates (for the contrast loss>loss avoidance) across voxels within a 10 mm diameter sphere, centered at peak coordinates (−18, −18, −20). ADM/BDM, patients scanned after/before the daily methadone intake; dAC, dorsal anterior cingulate; MB, midbrain; MB/PH, midbrain/parahippocampal gyrus. Regions significant at p<0.05 whole brain corrected. Error bars denote SEM.
At the anticipation/decision time of the task, for the contrast loss vs. neutral, both controls and MMT patients activated the insula/inferior frontal gyrus and the dorsal anterior cingulate (Figure 5a and b, Supplementary Table S11). A significant between-group difference was found in the left insula/inferior frontal gyrus ((−50, 20, −6), t=3.46) with patients exhibiting reduced discrimination between loss and neutral trials in this region. There was no significant difference in insula activity for the comparison ADM vs BDM, suggesting that both groups of patients contributed similarly to the difference between patients and controls for this brain region (Figure 5d, Supplementary Table S12).
Neural responses for the contrast loss>neutral at the decision time of the task. Both controls (a) and patients (b) activated the bilateral insula/inferior frontal gyrus and the dorsal anterior cingulate for the contrast loss>neutral at the decision time of the task. (c) Controls showed stronger neural responses than patients in the left insula/inferior frontal gyrus. (d) Mean value of parameter estimates across voxels within a 10 mm diameter sphere, centered at peak coordinates (−50, 20, −6) of the left insula/inferior frontal gyrus region where patients differed significantly from controls. ADM/BDM, patients scanned after/before the daily methadone intake; IN/IFG, insula/inferior frontal gyrus. Regions significant at p<0.05 whole brain corrected. Error bars denote SEM.
DISCUSSION
This study investigated the neural correlates of reward and loss processing in opiate-dependent patients receiving MMT. In accord with hypotheses, patients differed from controls in their neural responses to rewarding and aversive events.
On reward trials, controls exhibited discriminatory activation in the dorsal caudate for the outcomes win vs no-win, a pattern that was not observed in patients. This activation in controls is consistent with studies reporting the involvement of the caudate in reward processing (Delgado et al, 2005; Pizzagalli et al, 2009). In drug dependency, the dorsal caudate is implicated in compulsive drug seeking and habit formation (Everitt et al, 2008; Koob and Volkow, 2010). Our finding is consistent with studies reporting decreased neural sensitivity in drug-dependent patients for nondrug-related rewarding stimuli (Buhler et al, 2010; Diekhof et al, 2008; Goldstein et al, 2007; Peters et al, 2011; Wrase et al, 2007) and with a hypothesis of nondrug rewards being undervalued in drug dependency (Hyman et al, 2006).
During both reward and loss trials, controls activated the ventral striatum at the outcome time (for the contrasts win vs no-win and loss avoidance vs loss). This suggests that the ventral striatum represented loss avoidance similarly to reward events, consistent with previous findings (Pessiglione et al, 2006). In contrast to controls, during loss trials, patients failed to differentiate with regard to ventral striatal activity, between avoiding a loss and receiving a loss, resulting in significant between-group differences. This suggests a representational deficit in the ventral striatum of patients in processing aversive outcome information. The finding is consistent with a study reporting blunted striatal activation during the anticipation of loss in detoxified alcohol-dependent participants (Wrase et al, 2007).
During reward processing, activity in the ventral striatum has often been linked to the firing of dopaminergic neurons (O'Doherty et al, 2004). Ventral striatal activation during aversive processing may also relate to dopaminergic neuronal activity (Delgado et al, 2008). If so, the finding of altered ventral striatal activation during aversive processing could reflect abnormal functioning of the dopaminergic system in MMT patients, consistent with studies reporting decreased dopaminergic function and reduced D2 receptors in the striatum of addicted patients (Volkow et al, 2009). Alternatively, ventral striatal activity during aversive processing may also relate to alterations within other neurotransmitter systems (Delgado et al, 2008).
On loss trials at the decision time, patients exhibited decreased left insula/inferior frontal gyrus activation during the presentation of loss vs neutral stimuli. Insula responsiveness to anticipated losses predicts a participant’s ability to learn to avoid losses (Samanez-Larkin et al, 2008), and insula activation predicts behavioral avoidance of high-risk options during decision making (Kuhnen and Knutson, 2005). In our study, decreased insula activation in patients during the anticipation of loss could indicate reduced valuation of aversive outcomes, conceivably resulting in less efficient adjustment of behavior to minimize risks and avoid failures. The finding is consistent with reduced activity in the insula of pathological gamblers during anticipation of losses (Balodis et al, 2012).
Patients scanned after their daily methadone dose exhibited increased neural discrimination between loss and loss avoidance outcomes in the midbrain/parahippocampal gyrus compared with those scanned before methadone. In addition, increased neural responses to loss>loss avoidance correlated with increased methadone dose across all patients, for the left midbrain/parahippocampal gyrus. Both findings are consistent with methadone administration driving the increased activation. In this context, animal studies report that aversive stimuli causing conditioned place aversion can inhibit dopaminergic neurons in the ventral tegmental area (VTA) (Tan et al, 2012; Ungless et al, 2004). Aversive stimuli stimulate action potentials in GABAergic neurons in the VTA leading to inhibition of dopaminergic neurons (Tan et al, 2012). Opiates such as methadone activate μ-opioid receptors leading to hyperpolarisation of GABAergic neurons, with a reduction in GABA release onto dopaminergic neurons, reducing inhibition of dopamine firing (Matsui and Williams, 2011). Therefore, midbrain/parahippocampal gyrus activation in response to aversive stimuli could be due to disinhibition of dopaminergic activity. However, methadone may also disinhibit additional excitatory pathways in this brain region. Further work is required to clarify the increased signal observed in patients who had just taken their methadone and its significance for decision making.
Possible limitations of this study should be noted. Patients and controls differed with regard to IQ, symptoms of low mood, anxiety, and nicotine use. However, this was taken into account in the analysis, reproducing the findings while covarying for these variables (see Supplementary Material). It is important to note that the study design does not allow disentangling whether the observed brain abnormalities in patients relate to current methadone treatment, previous heroin addiction, or vulnerability to develop addiction.
In summary, this study investigated brain activity in response to rewarding and loss stimuli in opiate-dependent patients receiving MMT. Patients showed decreased responsiveness to rewarding stimuli in the dorsal caudate and decreased responsiveness to loss events in the ventral striatum and insula. The findings contribute to elucidating the neural correlates of the clinical features of opiate addiction, whereby drugs are pursued at the expense of nondrug-related life goals and despite adverse consequences. Our findings add further support to the suggestion that treatment for opiate addiction should aim to increase the reward value of nondrug-related reinforcers (Volkow et al, 2009) and highlight the importance of abnormalities in aversive information processing. Future studies are required to examine whether the observed neural abnormalities persist after long-term abstinence, predict relapse risk and relate to pre-morbid vulnerabilities.
FUNDING AND DISCLOSURE
This study was part funded by an unrestricted educational grant provided by Schering-Plough and a grant by an Anonymous Trust. The founding sources had no role in the design, conduct of the study and interpretation of the data. KM has Chaired advisory boards for studies of Deep Brain Stimulation for Obsessive-Compulsive Disorder sponsored by Medtronic. He has received educational grants from Cyberonics Inc. & Schering-Plough, and he has received research project funding from Merck Serono & Reckitt Benckiser and also from St Jude Medical for a multi-centre clinical trial of Deep Brain Stimulation for depression. He has received travel and accommodation support to attend meetings from Medtronic and St Jude Medical. JDS has received research funding via an honorarium associated with a lecture from Wyeth and an unrestricted educational grant from Schering-Plough. AB has received educational grants from Schering-Plough and he has received research project funding from Merck Serono and Reckitt Benckiser. DJKB has received research support from Vifor Pharma and a BBSRC Case award in collaboration with MSD and an honorarium from the Society for Research on Nicotine & Tobacco as Editor-in-Chief the Society’s research journal, Nicotine & Tobacco Research. VBG reported no biomedical financial interests or potential conflicts of interest.
References
Balodis IM, Kober H, Worhunsky PD, Stevens MC, Pearlson GD, Potenza MN (2012). Diminished frontostriatal activity during processing of monetary rewards and losses in pathological gambling. Biol Psychiatry 71: 749–757.
Berridge KC (2007). The debate over dopamine's role in reward: the case for incentive salience. Psychopharmacology 191: 391–431.
Buhler M, Vollstadt-Klein S, Kobiella A, Budde H, Reed LJ, Braus DF et al (2010). Nicotine dependence is characterized by disordered reward processing in a network driving motivation. Biol Psychiatry 67: 745–752.
Curran HV, Kleckham J, Bearn J, Strang J, Wanigaratne S (2001). Effects of methadone on cognition, mood and craving in detoxifying opiate addicts: a dose-response study. Psychopharmacology 154: 153–160.
Delgado MR, Li J, Schiller D, Phelps EA (2008). The role of the striatum in aversive learning and aversive prediction errors. Philos Trans R Soc Lond B Biol Sci 363: 3787–3800.
Delgado MR, Miller MM, Inati S, Phelps EA (2005). An fMRI study of reward-related probability learning. Neuroimage 24: 862–873.
Diekhof EK, Falkai P, Gruber O (2008). Functional neuroimaging of reward processing and decision-making: a review of aberrant motivational and affective processing in addiction and mood disorders. Brain Res Rev 59: 164–184.
Dyer KR, White JM (1997). Patterns of symptom complaints in methadone maintenance patients. Addiction 92: 1445–1455.
Everitt BJ, Belin D, Economidou D, Pelloux Y, Dalley JW, Robbins TW (2008). Review. Neural mechanisms underlying the vulnerability to develop compulsive drug-seeking habits and addiction. Philos Trans R Soc Lond B Biol Sci 363: 3125–3135.
Fehr C, Yakushev I, Hohmann N, Buchholz HG, Landvogt C, Deckers H et al (2008). Association of low striatal dopamine d2 receptor availability with nicotine dependence similar to that seen with other drugs of abuse. Am J Psychiatry 165: 507–514.
Garavan H, Pankiewicz J, Bloom A, Cho JK, Sperry L, Ross TJ et al (2000). Cue-induced cocaine craving: neuroanatomical specificity for drug users and drug stimuli. Am J Psychiatry 157: 1789–1798.
Goldstein RZ, Alia-Klein N, Tomasi D, Zhang L, Cottone LA, Maloney T et al (2007). Is decreased prefrontal cortical sensitivity to monetary reward associated with impaired motivation and self-control in cocaine addiction? Am J Psychiatry 164: 43–51.
Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO (1991). The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict 86: 1119–1127.
Heinz A, Siessmeier T, Wrase J, Hermann D, Klein S, Grusser SM et al (2004). Correlation between dopamine D(2) receptors in the ventral striatum and central processing of alcohol cues and craving. Am J Psychiatry 161: 1783–1789.
Hyman SE, Malenka RC, Nestler EJ (2006). Neural mechanisms of addiction: the role of reward-related learning and memory. Annu Rev Neurosci 29: 565–598.
Koob GF, Volkow ND (2010). Neurocircuitry of addiction. Neuropsychopharmacology 35: 217–238.
Kuhnen CM, Knutson B (2005). The neural basis of financial risk taking. Neuron 47: 763–770.
Langleben DD, Ruparel K, Elman I, Busch-Winokur S, Pratiwadi R, Loughead J et al (2008). Acute effect of methadone maintenance dose on brain FMRI response to heroin-related cues. Am J Psychiatry 165: 390–394.
Liu X, Hairston J, Schrier M, Fan J (2011). Common and distinct networks underlying reward valence and processing stages: a meta-analysis of functional neuroimaging studies. Neurosci Biobehav Rev 35: 1219–1236.
Martin-Soelch C, Chevalley AF, Kunig G, Missimer J, Magyar S, Mino A et al (2001). Changes in reward-induced brain activation in opiate addicts. Eur J Neurosci 14: 1360–1368.
Matsui A, Williams JT (2011). Opioid-sensitive GABA inputs from rostromedial tegmental nucleus synapse onto midbrain dopamine neurons. J Neurosci 31: 17729–17735.
Montague PR, Dayan P, Sejnowski TJ (1996). A framework for mesencephalic dopamine systems based on predictive Hebbian learning. J Neurosci 16: 1936–1947.
Nelson HE, Wilson JR (1991) The revised national adult reading test—test manual edn NFER-Wilson: Winsor.
Niv Y, Edlund JA, Dayan P, O'Doherty JP (2012). Neural prediction errors reveal a risk-sensitive reinforcement-learning process in the human brain. J Neurosci 32: 551–562.
O'Doherty J, Dayan P, Schultz J, Deichmann R, Friston K, Dolan RJ (2004). Dissociable roles of ventral and dorsal striatum in instrumental conditioning. Science 304: 452–454.
Pessiglione M, Seymour B, Flandin G, Dolan RJ, Frith CD (2006). Dopamine-dependent prediction errors underpin reward-seeking behaviour in humans. Nature 442: 1042–1045.
Peters J, Bromberg U, Schneider S, Brassen S, Menz M, Banaschewski T et al (2011). Lower ventral striatal activation during reward anticipation in adolescent smokers. Am J Psychiatry 168: 540–549.
Pizzagalli DA, Holmes AJ, Dillon DG, Goetz EL, Birk JL, Bogdan R et al (2009). Reduced caudate and nucleus accumbens response to rewards in unmedicated individuals with major depressive disorder. Am J Psychiatry 166: 702–710.
Samanez-Larkin GR, Hollon NG, Carstensen LL, Knutson B (2008). Individual differences in insular sensitivity during loss anticipation predict avoidance learning. Psychol Sci 19: 320–323.
Schultz W (1998). Predictive reward signal of dopamine neurons. J Neurophysiol 80: 1–27.
Sell LA, Morris JS, Bearn J, Frackowiak RS, Friston KJ, Dolan RJ (2000). Neural responses associated with cue evoked emotional states and heroin in opiate addicts. Drug Alcohol Depend 60: 207–216.
Slotnick SD, Moo LR, Segal JB, Hart J Jr. (2003). Distinct prefrontal cortex activity associated with item memory and source memory for visual shapes. Brain Res Cogn Brain Res 17: 75–82.
Tan KR, Yvon C, Turiault M, Mirzabekov JJ, Doehner J, Labouebe G et al (2012). GABA neurons of the VTA drive conditioned place aversion. Neuron 73: 1173–1183.
Ungless MA, Magill PJ, Bolam JP (2004). Uniform inhibition of dopamine neurons in the ventral tegmental area by aversive stimuli. Science 303: 2040–2042.
Volkow ND, Fowler JS, Wang GJ, Baler R, Telang F (2009). Imaging dopamine's role in drug abuse and addiction. Neuropharmacology 56: 3–8.
Wang GJ, Volkow ND, Fowler JS, Logan J, Abumrad NN, Hitzemann RJ et al (1997). Dopamine D2 receptor availability in opiate-dependent subjects before and after naloxone-precipitated withdrawal. Neuropsychopharmacology 16: 174–182.
Wrase J, Schlagenhauf F, Kienast T, Wustenberg T, Bermpohl F, Kahnt T et al (2007). Dysfunction of reward processing correlates with alcohol craving in detoxified alcoholics. Neuroimage 35: 787–794.
Wrase J, Schlagenhauf F, Kienast T, Wustenberg T, Bermpohl F, Kahnt T et al (2006). Dysfunction of reward processing correlates with alcohol craving in detoxified alcoholics. Neuroimage 35: 787–794.
Zigmond AS, Snaith RP (1983). The hospital anxiety and depression scale. Acta Psychiatr Scand 67: 361–370.
Acknowledgements
The study was adopted and supported by staff funded by the Scottish Mental Health Research Network. We thank the NHS Fife Research and Development Department and NHS Fife Addiction Services for their support in the recruitment, especially Sarah Gray, Angela Swift, Dawn Stewart, Michelle Hyslop, Anthony Robb, and Fiona Boyce together with all clinical staff. Christine Matthews, Mairi Stirling, and Craig Adams helped with data management. Dr Jennifer McFarlane, Dr Ian Cavin, and Dr Gordon Waiter advised on fMRI design and data acquisition. Professor Tim Hales provided helpful discussions on neurobiology.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
Supplementary information
Rights and permissions
About this article
Cite this article
Gradin, V., Baldacchino, A., Balfour, D. et al. Abnormal Brain Activity During a Reward and Loss Task in Opiate-Dependent Patients Receiving Methadone Maintenance Therapy. Neuropsychopharmacol 39, 885–894 (2014). https://doi.org/10.1038/npp.2013.289
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2013.289
Keywords
This article is cited by
-
A Systematic Review on Common and Distinct Neural Correlates of Risk-taking in Substance-related and Non-substance Related Addictions
Neuropsychology Review (2023)
-
Brain network dysfunctions in addiction: a meta-analysis of resting-state functional connectivity
Translational Psychiatry (2022)
-
The neurobiology of drug addiction: cross-species insights into the dysfunction and recovery of the prefrontal cortex
Neuropsychopharmacology (2022)
-
Protracted abstinence in males with an opioid use disorder: partial recovery of nucleus accumbens function
Translational Psychiatry (2022)
-
Computational Mechanisms of Addiction: Recent Evidence and Its Relevance to Addiction Medicine
Current Addiction Reports (2021)