Key Points
-
Migraine is a common and often disabling disorder that is increasingly being recognized as a fundamentally neurological problem.
-
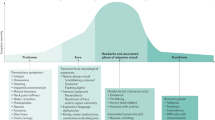
Brain-imaging data indicate that the brainstem is pivotal in the pathophysiology of the disorder and, together with the electrophysiological data and the pan-sensory disturbance, a dysfunction of the thalamic processing of afferent traffic is a plausible way of explaining a large part of the problem.
-
For pain processing, the trigeminocervical complex is pivotal and provides an attractive entirely neural target for therapy.
-
This review describes why migraine is a central nervous system problem, and discusses the main approaches that will lead to non-vascular neurally acting treatments for this common and important neurological condition.
-
The potential targets for such an action include calcitonin gene-related peptide (CGRP) receptors, 5-HT1F and 5-HT1D receptors, glutamate receptors, adenosine A1 receptors, nociceptin, vanilloid transient-receptor potential V1 (TRPV1) receptors, cannabinoid CB1 receptors, orexin receptors and nitric oxide (NO)-based mechanisms.
Abstract
Serotonin (5-HT)1B/1D receptor agonists, which are also known as triptans, represent the most important advance in migraine therapeutics in the four millennia that the condition has been recognized. The vasoconstrictive activity of triptans produced a small clinical penalty in terms of coronary vasoconstriction but also raised an enormous intellectual question: to what extent is migraine a vascular problem? Functional neuroimaging and neurophysiological studies have consistently developed the theme of migraine as a brain disorder and, therefore, demanded that the search for neurally acting antimigraine drugs should be undertaken. The prospect of non-vasoconstrictor acute migraine therapies, potential targets for which are discussed here, offers a real opportunity to patients and provides a therapeutic rationale that places migraine firmly in the brain as a neurological problem, where it undoubtedly belongs.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Lipton, R. B., Stewart, W. F., Diamond, S., Diamond, M. L. & Reed, M. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache 41, 646–657 (2001).
Menken, M., Munsat, T. L. & Toole, J. F. The global burden of disease study: implications for neurology. Arch. Neurol. 57, 418–420 (2000).
Goadsby, P. J., Lipton, R. B. & Ferrari, M. D. Migraine: current understanding and treatment. N. Engl. J. Med. 346, 257–270 (2002). An overall review of migraine pathophysiology and treatment.
Lance, J. W. & Goadsby, P. J. Mechanism and Management of Headache (Elsevier, New York, 2005). The latest (seventh) edition of a popular book with an overview of headache.
Goadsby, P. J. The pharmacology of headache. Prog. Neurobiol. 62, 509–525 (2000).
Doenicke, A., Siegel, E., Hadoke, M. & Perrin, V. L. Initial clinical study of AH25086B (5-HT1-like agonist) in the acute treatment of migraine. Cephalalgia 7, 437–438 (1987).
Doenicke, A., Brand, J. & Perrin, V. L. Possible benefit of GR43175, a novel 5-HT1-like receptor agonist, for the acute treatment of severe migraine. Lancet 1, 1309–1311 (1988).
Ferrari, M. D. & The Subcutaneous Sumatriptan International Study Group. Treatment of migraine attacks with sumatriptan. N. Engl. J. Med. 325, 316–321 (1991).
Dodick, D. et al. Consensus statement: cardiovascular safety profile of triptans (5-HT1B/1D agonists) in the acute treatment of migraine. Headache 44, 414–425 (2004).
Ferrari, M. D., Roon, K. I., Lipton, R. B. & Goadsby, P. J. Oral triptans (serotonin, 5-HT1B/1D agonists) in acute migraine treatment: a meta-analysis of 53 trials. Lancet 358, 1668–1675 (2001). This paper compares the main triptans according to their efficacy and side effect endpoints.
Ferrari, M. D., Goadsby, P. J., Roon, K. I. & Lipton, R. B. Triptans (serotonin, 5-HT1B/1D agonists) in migraine: detailed results and methods of a meta-analysis of 53 trials. Cephalalgia 22, 633–658 (2002).
Goadsby, P. J. Post-triptan era for the treatment of acute migraine. Curr. Pain Headache Rep. 8, 393–398 (2004).
Cohen, A. S. & Goadsby, P. J. Functional neuroimaging of primary headache disorders. Curr. Neurol. Neurosci. Rep. 4, 105–110 (2004).
Hadjikhani, N. et al. Mechanisms of migraine aura revealed by functional MRI in human visual cortex. Proc. Natl Acad. Sci. USA 98, 4687–4692 (2001). An important paper that images migraine aura and provides compelling evidence for its similarity to CSD.
Kaube, H. & Giffin, N. J. The electrophysiology of migraine. Curr. Opin. Neurol. 15, 303–309 (2002).
Ambrosini, A. & Schoenen, J. The electrophysiology of migraine. Curr. Opin. Neurol. 16, 327–331 (2003).
Weiller, C. et al. Brain stem activation in spontaneous human migraine attacks. Nature Med. 1, 658–660 (1995).
Welch, K. M., Nagesh, V., Aurora, S. & Gelman, N. Periaqueductal grey matter dysfunction in migraine: cause or the burden of illness? Headache 41, 629–637 (2001).
Goadsby, P. J. Neurovascular headache and a midbrain vascular malformation: evidence for a role of the brainstem in chronic migraine. Cephalalgia 22, 107–111 (2002).
Haas, D. C., Kent, P. F. & Friedman, D. I. Headache caused by a single lesion of multiple sclerosis in the periaqueductal gray area. Headache 33, 452–455 (1993).
Raskin, N. H., Hosobuchi, Y. & Lamb, S. Headache may arise from perturbation of brain. Headache 27, 416–420 (1987).
Veloso, F., Kumar, K. & Toth, C. Headache secondary to deep brain implantation. Headache 38, 507–515 (1998).
Knight, Y. E. & Goadsby, P. J. The periaqueductal gray matter modulates trigeminovascular input: a role in migraine? Neuroscience 106, 793–800 (2001).
Knight, Y. E., Bartsch, T. & Goadsby, P. J. Trigeminal antinociception induced by bicuculline in the periaqueductal grey (PAG) is not affected by PAG P/Q-type calcium channel blockade in rat. Neurosci. Lett. 336, 113–116 (2003).
Knight, Y. E., Bartsch, T., Kaube, H. & Goadsby, P. J. P/Q-type calcium channel blockade in the PAG facilitates trigeminal nociception: a functional genetic link for migraine? J. Neurosci. 22, 1–6 (2002). This important paper illustrates the principle that brain dysfunction without peripheral change can produce alterations in pain-pathway function.
Bandler, R. & Keay, K. A. Columnar organization in the midbrain periaqueductal gray and the integration of emotional expression. Progress Brain Res. 107, 285–300 (1996).
Bartsch, T., Knight, Y. E. & Goadsby, P. J. Activation of 5-HT1B/1D receptors in the periaqueductal grey inhibits meningeal nociception. Ann. Neurol. 56, 371–381 (2004). An extremely important paper that provides a new possible locus of action for triptans and opens up the possibility of a non-trigeminal function.
Afridi, S. & Goadsby, P. J. New onset migraine with a brainstem cavernous angioma. J. Neurol. Neurosurg. Psychiatr. 74, 680–682 (2003).
Bahra, A., Matharu, M. S., Buchel, C., Frackowiak, R. S. J. & Goadsby, P. J. Brainstem activation specific to migraine headache. Lancet 357, 1016–1017 (2001).
Afridi, S. et al. A PET study exploring the laterality of brainstem activation in migraine using glyceryl trinitrate. Cephalalgia 24, 775–776 (2004).
Afridi, S. et al. A PET study in spontaneous migraine. Arch. Neurol. 62, 1270–1275 (2005).
Amaral, D. G. & Sinnamon, H. M. The locus coeruleus: neurobiology of a central noradrenergic nucleus. Prog. Neurobiol. 9, 147–196 (1977).
Goadsby, P. J., Lambert, G. A. & Lance, J. W. Differential effects on the internal and external carotid circulation of the monkey evoked by locus coeruleus stimulation. Brain Res. 249, 247–254 (1982).
Goadsby, P. J. & Duckworth, J. W. Low frequency stimulation of the locus coeruleus reduces regional cerebral blood flow in the spinalized cat. Brain Res. 476, 71–77 (1989).
May, A., Bahra, A., Buchel, C., Frackowiak, R. S. J. & Goadsby, P. J. Hypothalamic activation in cluster headache attacks. Lancet 352, 275–278 (1998). This was the first paper to show posterior hypothalamic region activity in cluster headache.
May, A. et al. Experimental cranial pain elicited by capsaicin: a PET-study. Pain 74, 61–66 (1998).
Tracey, I. et al. Imaging attentional modulation of pain in the periaqueductal gray in humans. J. Neurosci. 22, 2748–2752 (2002).
Schoenen, J., Ambrosini, A., Sandor, P. S. & Maertens de Noordhout, A. Evoked potentials and transcranial magnetic stimulation in migraine: published data and viewpoint on their pathophysiologic significance. Clin. Neurophysiol. 114, 955–972 (2003).
Afra, J., Sandor, P. & Schoenen, J. Habituation of visual and intensity dependence of cortical auditory evoked potentials tend to normalise just before and during migraine attacks. Cephalalgia 20, 347 (2000).
Proietti-Cecchini, A., Afra, J. & Schoenen, J. Intensity dependence of the cortical auditory evoked potentials as a surrogate marker of central nervous system serotonin transmission in man: demonstration of a central effect for the 5HT1B/1D agonist zolmitriptan (311C90, Zomig). Cephalalgia 17, 849–854 (1997).
Schoenen, J., Wang, W., Albert, A. & Delwaide, P. J. Potentiation instead of habituation characterizes visual evoked potentials in migraine patients between attacks. Eur. J. Neurol. 2, 115–122 (1995).
Wang, W. & Schoenen, J. Interictal potentiation of passive 'oddball' auditory event-related potentials in migraine. Cephalalgia 18, 261–265 (1998). This important paper illustrates the typical electrophysiological defect in migraine dyshabituation.
Niebur, E., Hsiao, S. S. & Johnson, K. O. Synchrony: a neural mechanism for attentional selection? Curr. Opin. Neurobiol. 12, 190–194 (2002). This fascinating paper sets out the possible mechanisms for neural synchrony.
Angelini, L. et al. Steady-state visual evoked potentials and phase synchronization in migraine patients. Phys. Rev. Lett. 93, 038103-1–038103-4 (2004).
Goadsby, P. J. Migraine pathophysiology: the brainstem governs the cortex. Cephalalgia 23, 565–566 (2003).
Schoenen, J. & Timsit-Berthier, M. Contingent negative variation: methods and potential interest in headache. Cephalalgia 13, 28–32 (1993).
Kropp, P. & Gerber, W. D. Prediction of migraine attacks using a slow cortical potential, the contingent negative variation. Neurosci. Lett. 257, 73–76 (1998).
Maertens de Noordhout, A., Timsit-Berthier, M. & Schoenen, J. Contingent negative variation (CNV) in migraineurs before and during prophylactic treatment with β-blockers. Cephalalgia 5, 34–35 (1985). This important paper illustrates an electrophysiological trait of migraine that can be reversed by a preventive treatment.
Gantenbein, A., Goadsby, P. J. & Kaube, H. Introduction of a clinical scoring system for migraine research applied to electrophysiological studies. Cephalalgia 24, 1095–1096 (2004).
Headache Classification Committee of The International Headache Society. The International Classification of Headache Disorders (second edition). Cephalalgia 24, 1–160 (2004). This paper gives contemporary definitions for all headache types.
Olesen, J. et al. Timing and topography of cerebral blood flow, aura, and headache during migraine attacks. Ann. Neurol. 28, 791–798 (1990). A ground-breaking observation of blood-flow changes in migraine with aura that led to the spreading depression hypothesis.
Cutrer, F. M. et al. Perfusion-weighted imaging defects during spontaneous migrainous aura. Ann. Neurol. 43, 25–31 (1998). This extremely important observation expanded on earlier flow work and led to a non-ambiguous method that confirmed spreading depression as the substrate for migraine aura.
Leao, A. A. P. Spreading depression of activity in cerebral cortex. J. Neurophysiol. 7, 359–390 (1944).
Leao, A. A. P. Pial circulation and spreading activity in the cerebral cortex. J. Neurophysiol. 7, 391–396 (1944).
Lauritzen, M. Pathophysiology of the migraine aura. The spreading depression theory. Brain 117, 199–210 (1994).
Moskowitz, M. A., Bolay, H. & Dalkara, T. Deciphering migraine mechanisms: clues from familial hemiplegic migraine genotypes. Ann. Neurol. 55, 276–280 (2004).
Goadsby, P. J. Migraine, aura and cortical spreading depression: why are we still talking about it? Ann. Neurol. 49, 4–6 (2001).
De Vries, P., Villalon, C. M. & Saxena, P. R. Pharmacological aspects of experimental headache models in relation to acute antimigraine therapy. Eur. J. Pharmacol. 375, 61–74 (1999).
Goadsby, P. J. & Kaube, H. in The Headaches 2nd edn (eds Olesen, J., Tfelt-Hansen, P. & Welch, K. M. A.) 195–202 (Lippincott Williams & Wilkins, Philadelphia, 2000).
Saxena, P. R. & De Boer, M. O. Pharmacology of antimigraine drugs. J. Neurol. 238, S28–S35 (1991).
Saxena, P. R. & Cairo-Rawlins, W. I. Presynaptic inhibition by ergotamine of the responses to cardioaccelerator nerve stimulations in the cat. Eur. J. Pharmacol. 58, 305–312 (1979).
Markowitz, S., Saito, K. & Moskowitz, M. A. Neurogenically mediated leakage of plasma proteins occurs from blood vessels in dura mater but not brain. J. Neurosci. 7, 4129–4136 (1987).
Markowitz, S., Saito, K. & Moskowitz, M. A. Neurogenically mediated plasma extravasation in dura mater: effect of ergot alkaloids. A possible mechanism of action in vascular headache. Cephalalgia 8, 83–91 (1988).
Williamson, D. J., Hargreaves, R. J., Hill, R. G. & Shepheard, S. L. Sumatriptan inhibits neurogenic vasodilation of dural blood vessels in the anaesthetized rat- intravital microscope studies. Cephalalgia 17, 525–531 (1997).
Kaube, H., Hoskin, K. L. & Goadsby, P. J. Activation of the trigeminovascular system by mechanical distension of the superior sagittal sinus in the cat. Cephalalgia 12, 133–136 (1992).
Burstein, R. & Jakubowski, M. Analgesic triptan action in an animal model of intracranial pain: a race against the development of central sensitisation. Ann. Neurol. 55, 27–36 (2004).
Selby, G. & Lance, J. W. Observations on 500 cases of migraine and allied vascular headache. J. Neurol. Neurosurg. Psychiatr. 23, 23–32 (1960).
Tfelt-Hansen, P. et al. Ergotamine in the acute treatment of migraine: a review and European consensus. Brain 123, 9–18 (2000).
Buzzi, M. G. & Moskowitz, M. A. Evidence for 5-HT1B/1D receptors mediating the antimigraine effect of sumatriptan and dihydroergotamine. Cephalalgia 11, 165–168 (1991).
Hoskin, K. L., Kaube, H. & Goadsby, P. J. Central activation of the trigeminovascular pathway in the cat is inhibited by dihydroergotamine. A c-Fos and electrophysiology study. Brain 119, 249–256 (1996).
Read, S. J., Smith, M. I., Hunter, A. J., Upton, N. & Parsons, A. A. SB-220453, a potential novel antimigraine compound, inhibits nitric oxide release following induction of cortical spreading depression in the anaesthetized cat. Cephalalgia 20, 92–99 (1999).
Smith, M. I. et al. Repetitive cortical spreading depression in a gyrencephalic feline brain: inhibition by the novel benzoylamino-benzopyran SB-220453. Cephalalgia 20, 546–53 (2000).
MaassenVanDenBrink, A. et al. The potential anti-migraine compound SB-220453 does not contract human isolated blood vessels or myocardium; a comparison with sumatriptan. Cephalalgia 20, 538–545 (2000).
Parsons, A. A. et al. Tonabersat (SB-220453) a novel benzopyran with anticonvulsant properties attenuates trigeminal nerve-induced neurovascular reflexes. Br. J. Pharmacol. 132, 1549–1557 (2001).
Diener, H. C. et al. Topiramate in migraine prophylaxis: results from a placebo-controlled trial with propranolol as an active control. J. Neurol. 251, 943–950 (2004).
Brandes, J. L. et al. Topiramate for migraine prevention: a randomized controlled trial. JAMA 291, 965–973 (2004).
Silberstein, S. D., Neto, W., Schmitt, J. & Jacobs, D. Topiramate in migraine prevention: results of a large controlled trial. Arch. Neurol. 61, 490–495 (2004).
Akerman, S. & Goadsby, P. J. Topiramate inhibits cortical spreading depression in rat and cat: a possible contribution to its preventive effect in migraine. Cephalalgia 24, 783–784 (2004).
Tvedskov, J. F., Iversen, H. K. & Olesen, J. A double-blind study of SB-220453 (Tonerbasat) in the glyceryltrinitrate (GTN) model of migraine. Cephalalgia 24, 875–882 (2004).
Tvedskov, J. F. et al. The effect of propranolol on glyceryltrinitrate-induced headache and arterial response. Cephalalgia 24, 1076–1087 (2004).
Tvedskov, J. F. et al. The prophylactic effect of valproate on glyceryltrinitrate induced migraine. Cephalalgia 24, 576–585 (2004).
Storer, R. J. & Goadsby, P. J. Topiramate inhibits trigeminovascular neurons in the cat. Cephalalgia 24, 1049–1056 (2004).
Ophoff, R. A. et al. Familial hemiplegic migraine and episodic ataxia type-2 are caused by mutations in the Ca2+ channel gene CACNL1A4. Cell 87, 543–552 (1996). This ground-breaking report of the first clear genetic defect in a migraine syndrome pointed to the principle of migraine as a channelopathy.
van den Maagdenberg, A. M. J. M. et al. A Cacna1a knock-in migraine mouse model with increased susceptibility to cortical spreading depression. Neuron 41, 701–710 (2004). An excellent example of a translational work that shows the effects of a human mutation in a mouse model.
Shank, R. P., Gardocki, J. F., Streeter, A. J. & Maryanoff, B. E. An overview of the preclinical aspects of topiramate: pharmacology, pharmacokinetics, and mechanism of action. Epilepsia 41, S3–S9 (2000).
Geer, J. J., Dooley, D. J. & Adams, M. E. K(+)-stimulated 45Ca2+ flux into rat neocortical mini-slices is blocked by omega-Aga-IVA and the dual Na+/Ca2+ channel blockers lidoflazine and flunarizine. Neurosci. Lett. 158, 97–100 (1993).
Ebersberger, A., Portz, S., Meissner, W., Schaible, H. G. & Richter, F. Effects of N-, P/Q- and L-type calcium channel blockers on nociceptive neurones of the trigeminal nucleus with input from the dura. Cephalalgia 24, 250–261 (2004).
Shields, K. G., Storer, R. J., Akerman, S. & Goadsby, P. J. Calcium channels modulate nociceptive transmission in the trigeminal nucleus of the cat. Neuroscience (in the press).
Akerman, S., Williamson, D. & Goadsby, P. J. Voltage-dependent calcium channels are involved in neurogenic dural vasodilation via a pre-synaptic transmitter release mechanism. Br. J. Pharmacol. 140, 558–566 (2003).
Kimball, R. W., Friedman, A. P. & Vallejo, E. Effect of serotonin in migraine patients. Neurology 10, 107–111 (1960).
Lance, J. W., Anthony, M. & Hinterberger, H. The control of cranial arteries by humoral mechanisms and its relation to the migraine syndrome. Headache 7, 93–102 (1967).
Humphrey, P. P. A. et al. Serotonin and migraine. Ann. NY Acad. Sci. 600, 587–598 (1990). This paper presents a good summary of the development of sumatriptan from the perspective of the inventors.
Lance, J. W., Fine, R. D. & Curran, D. A. An evaluation of methysergide in the prevention of migraine and other vascular headache. Med. J. Aust. 1, 814–818 (1963).
Johnston, B. M. & Saxena, P. R. The effect of ergotamine on tissue blood flow and the arteriovenous shunting of radioactive microspheres in the head. Br. J. Pharmacol. 63, 541–549 (1978).
Phebus, L. A. et al. Characterization of LY334370 as a pharmacological tool to study 5HT1F receptors- binding affinities, brain penetration and activity in the neurogenic dural inflammation model of migraine. Life Sci. 61, 2117–2126 (1997).
Johnson, K. W. et al. 5-HT1F receptor agonists inhibit neurogenic dural inflammation in guinea pigs. NeuroReport 8, 2237–2240 (1997).
Cohen, M. L. & Schenck, K. 5-Hydroxytryptamine(1F) receptors do not participate in vasoconstriction: lack of vasoconstriction to LY344864, a selective serotonin(1F) receptor agonist in rabbit saphenous vein. J. Pharmacol. Exp. Ther. 290, 935–939 (1999).
Razzaque, Z. et al. Vasoconstriction in human isolated middle meningeal arteries: determining the contribution of 5-HT1B- and 5-HT1F-receptor activation. Br. J. Clin. Pharmacol. 47, 75–82 (1999).
Goldstein, D. J. et al. Selective serotonin 1F (5-HT(1F)) receptor agonist LY334370 for acute migraine: a randomised controlled trial. Lancet 358, 1230–1234 (2001). This was the first clinical study of a 5-HT 1F receptor agonist in migraine.
Castro, M. E. et al. Differential distribution of [3H]sumatriptan binding sites (5-HT1B, 5-HT1D and 5-HT1F receptors) in human brain: focus on brainstem and spinal cord. Neuropharmacology 36, 535–542 (1997).
Pascual, J., Arco, C. D., Romon, T., Olmo, C. D. & Pazos, A. [3H] Sumatriptan binding sites in human brain: regional-dependent labelling of 5HT1D and 5HT1F receptors. Eur. J. Pharmacol. 295, 271–274 (1996).
Waeber, C. & Moskowitz, M. A. [3H]sumatriptan labels both 5-HT1D and 5HT1F receptor bindings sites in the guinea pig brain: an autoradiographic study. Naunyn Schmiedebergs Arch. Pharmacol. 352, 263–275 (1995).
Fugelli, A., Moret, C. & Fillion, G. Autoradiographic localization of 5-HT1E and 5-HT1F binding sites in rat brain: effect of serotonergic lesioning. J. Recept. Sig. Transduct. Res. 17, 631–645 (1997).
Bouchelet, I., Cohen, Z., Case, B. & Hamel, E. Differential expression of sumatriptan-sensitive 5-hydroxytryptamine receptors in human trigeminal ganglia and cerebral blood vessels. Mol. Pharmacol. 50, 219–223 (1996).
Mitsikostas, D. D., Sanchez del Rio, M., Moskowitz, M. A. & Waeber, C. Both 5-HT1B and 5-HT1F receptors modulate c-fos expression within rat trigeminal nucleus caudalis. Eur. J. Pharmacol. 369, 271–277 (1999).
Goadsby, P. J. & Classey, J. D. Evidence for 5-HT1B, 5-HT1D and 5-HT1F receptor inhibitory effects on trigeminal neurons with craniovascular input. Neuroscience 122, 491–498 (2003). This study dissects out the contribution of 5-HT 1B , 5-HT 1D and 5-HT 1F receptors to the inhibition of trigeminovascular neurons.
Maneesi, S., Akerman, S., Lasalandra, M. P., Classey, J. D. & Goadsby, P. J. Electron microscopic demonstration of pre- and postsynaptic 5-HT1D and 5-HT1F receptor immunoreactivity (IR) in the rat trigeminocervical complex (TCC) new therapeutic possibilities for the triptans. Cephalalgia 24, 148 (2004).
McCall, R. B. et al. Preclinical studies characterizing the anti-migraine and cardiovascular effects of the selective 5-HT 1D receptor agonist PNU-142633. Cephalalgia 22, 799–806 (2002).
McCall, R. B. Trigeminal ganglion elicited increases in nucleus trigeminal caudalis blood flow: a novel migraine model. Brain Res. 775, 189–192 (1997).
Waeber, C., Cutrer, F. M., Yu, X.-J. & Moskowitz, M. A. The selective 5HT1D receptor agonist U-109291 blocks dural plasma extravasation and c-fos expression in the trigeminal nucleus caudalis. Cephalalgia 17, 401 (1997).
Potrebic, S., Ahan, A. H., Skinner, K., Fields, H. L. & Basbaum, A. I. Peptidergic nociceptors of both trigeminal and dorsal root ganglia express serotonin 1D receptors: implications for the selective antimigraine action of triptans. J. Neurosci. 23, 10988–10997 (2003).
Ahn, A. H., Fields, H. L. & Basbaum, A. I. The triptan receptor 5HT1D is dynamically regulated in the central terminal of primary afferents in models of pain. Neurology 62, A440–A441 (2004). This abstract introduced the concept of the use-dependent expression of 5-HT 1D receptors.
Pregenzer, J. F., Alberts, G. L., Block, J. H., Slightom, J. L. & Im, W. B. Characterisation of ligand binding properties of the 5-HT1D receptors cloned from chimpanzee, gorilla and rhesus monkey in comparison with those from the human and guinea pig receptors. Neurosci. Lett. 235, 117–120 (1997).
Gomez-Mancilla, B. et al. Safety and efficacy of PNU-142633, a selective 5-HT1D agonist, in patients with acute migraine. Cephalalgia 21, 727–732 (2001).
Pregenzer, J. F. et al. Differential pharmacology between the guinea-pig and the gorilla 5-HT1D receptor as probed with isochromans (5-HT1D-selective ligands). Br. J. Pharmacol. 127, 468–472 (1999).
Fleishaker, J. C. et al. Pharmacokinetics and tolerability of a novel 5-HT1D agonist, PNU- 142633F. Int. J. Clin. Pharmacol. Ther. 37, 487–492 (1999).
Clements, J. R., Magnusson, K. R., Hautman, J. & Beitz, A. J. Rat tooth pulp projections to spinal trigeminal subnucleus caudalis are glutamate-like immunoreactive. J. Comp. Neurol. 309, 281–288 (1991).
Magnusson, K. R., Larson, A. A., Madl, J. E., Altschuler, R. A. & Beitz, A. J. Co-localization of fixative-modified glutamate and glutaminase in neurons of the spinal trigeminal nucleus of the rat: an immunohistochemical and immunoradiochemical analysis. J. Comp. Neurol. 247, 477–490 (1986).
Tallaksen-Greene, S. J., Young, A. B., Penney, J. B. & Beitz, A. J. Excitatory amino acid binding sites in the trigeminal principal sensory and spinal trigeminal nuclei of the rat. Neurosci. Lett. 141, 79–83 (1992).
Storer, R. J. & Goadsby, P. J. Trigeminovascular nociceptive transmission involves N-methyl-D-aspartate and non-N-methyl-D-aspartate glutamate receptors. Neuroscience 90, 1371–1376 (1999).
Goadsby, P. J. & Classey, J. D. Glutamatergic transmission in the trigeminal nucleus assessed with local blood flow. Brain Res. 875, 119–124 (2000).
Classey, J. D., Knight, Y. E. & Goadsby, P. J. The NMDA receptor antagonist MK-801 reduces Fos-like immunoreactivity within the trigeminocervical complex following superior sagittal sinus stimulation in the cat. Brain Res. 907, 117–124 (2001).
Mitsikostas, D. D., Sanchez del Rio, M., Waeber, C., Moskowitz, M. A. & Cutrer, F. M. The NMDA receptor antagonist MK-801 reduces capsaicin-induced c-fos expression within rat trigeminal nucleus caudalis. Pain 76, 239–248 (1998).
Mitsikostas, D. D. et al. Non-NMDA glutamate receptors modulate capsaicin induced c-fos expression within trigeminal nucleus caudalis. Br. J. Pharmacol. 127, 623–630 (1999).
Shields, K. G., Kaube, H. & Goadsby, P. J. GABA receptors modulate trigeminovascular nociceptive transmission in the ventroposteromedial (VPM) thalamic nucleus of the rat. Cephalalgia 23, 728 (2003).
Shields, K. G. & Goadsby, P. J. Propranolol modulates trigeminovascular responses in thalamic ventroposteromedial nucleus: a role in migraine? Brain 128, 86–97 (2005). This is an important description of the possible locus of action of the preventive propranolol in the thalamus.
Ramadan, N. M. et al. IV LY293558, an AMPA/kainate receptor antagonist, is effective in migraine. Cephalalgia 21, 267–268 (2001).
Kaube, H., Herzog, J., Kaufer, T., Dichgans, M. & Diener, H. C. Aura in some patients with familial hemiplegic migraine can be stopped by intranasal ketamine. Neurology 55, 139–141 (2000).
Edvinsson, L., Ekman, R., Jansen, I., McCulloch, J. & Uddman, R. Calcitonin gene-related peptide and cerebral blood vessels: distribution and vasomotor effects. J. Cereb. Blood Flow Metab. 7, 720–728 (1987).
Goadsby, P. J., Edvinsson, L. & Ekman, R. Release of vasoactive peptides in the extracerebral circulation of man and the cat during activation of the trigeminovascular system. Ann. Neurol. 23, 193–196 (1988).
Goadsby, P. J., Edvinsson, L. & Ekman, R. Vasoactive peptide release in the extracerebral circulation of humans during migraine headache. Ann. Neurol. 28, 183–187 (1990). This was the first description of CGRP and not substance-P release in migraine.
Gallai, V. et al. Vasoactive peptides levels in the plasma of young migraine patients with and without aura assessed both interictally and ictally. Cephalalgia 15, 384–390 (1995).
Goadsby, P. J. & Edvinsson, L. Human in vivo evidence for trigeminovascular activation in cluster headache. Brain 117, 427–434 (1994). This was the first description of CGRP release in cluster headache.
Fanciullacci, M., Alessandri, M., Figini, M., Geppetti, P. & Michelacci, S. Increase in plasma calcitonin gene-related peptide from extracerebral circulation during nitroglycerin-induced cluster headache attack. Pain 60, 119–123 (1995).
Thomsen, L. L., Kruuse, C., Iversen, H. K. & Olesen, J. A nitric oxide donor (nitroglycerine) triggers genuine migraine attacks. Eur. J. Neurol. 1, 73–80 (1994).
Afridi, S., Kaube, H. & Goadsby, P. J. Glyceryl trinitrate triggers premonitory symptoms in migraineurs. Pain 110, 675–680 (2004).
Juhasz, G. et al. NO-induced migraine attack: strong increase in plasma calcitonin gene-related peptide (CGRP) concentration and negative correlation with platelet serotonin release. Pain 106, 461–470 (2003).
Buzzi, M. G., Moskowitz, M. A., Shimizu, T. & Heath, H. H. Dihydroergotamine and sumatriptan attenuate levels of CGRP in plasma in rat superior sagittal sinus during electrical stimulation of the trigeminal ganglion. Neuropharmacology 30, 1193–1200 (1991).
Arvieu, L. et al. Sumatriptan inhibits the release of CGRP and substance P from the rat spinal cord. Neuroreport 7, 1973–1976 (1996).
Goadsby, P. J. & Edvinsson, L. Peripheral and central trigeminovascular activation in cat is blocked by the serotonin (5HT)-1D receptor agonist 311C90. Headache 34, 394–399 (1994).
Goadsby, P. J. & Edvinsson, L. The trigeminovascular system and migraine: studies characterizing cerebrovascular and neuropeptide changes seen in humans and cats. Ann. Neurol. 33, 48–56 (1993). This report showed that sumatriptan administration blocked CGRP release in migraine.
Zagami, A. S., Goadsby, P. J. & Edvinsson, L. Stimulation of the superior sagittal sinus in the cat causes release of vasoactive peptides. Neuropeptides 16, 69–75 (1990).
Knight, Y. E., Edvinsson, L. & Goadsby, P. J. Blockade of CGRP release after superior sagittal sinus stimulation in cat: a comparison of avitriptan and CP122, 288. Neuropeptides 33, 41–46 (1999).
Knight, Y. E., Edvinsson, L. & Goadsby, P. J. 4991W93 inhibits release of calcitonin gene-related peptide in the cat but only at doses with 5HT1B/1D receptor agonist activity. Neuropharmacology 40, 520–525 (2001).
Durham, P. L., Sharma, R. V. & Russo, A. F. Repression of the calcitonin gene-related peptide promoter by 5-HT1 receptor activation. J. Neurosci. 17, 9545–9553 (1997).
Durham, P. L. & Russo, A. F. Regulation of calcitonin gene-related peptide secretion by a serotonergic antimigraine drug. J. Neurosci. 19, 3423–3429 (1999).
Doods, H. et al. Pharmacological profile of BIBN4096BS, the first selective small molecule CGRP antagonist. Br. J. Pharmacol. 129, 420–423 (2000). This was the first description of a selective CGRP antagonist.
Moreno, M. J., Abounader, R., Hebert, E., Doods, H. & Hamel, E. Efficacy of the non-peptide CGRP receptor antagonist BIBN4096BS in blocking CGRP-induced dilations in human and bovine cerebral arteries: potential implications in acute migraine treatment. Neuropharmacology 42, 568–576 (2002).
Petersen, K. A., Lassen, L. H., Birk, S. & Olesen, J. The effect of the nonpeptide CGRP-antagonist, BIBN406BS on human-αCGRP induced headache and hemodynamics in healthy volunteers. Cephalalgia 23, 725 (2003).
Storer, R. J., Akerman, S. & Goadsby, P. J. Calcitonin gene-related peptide (CGRP) modulates nociceptive trigeminovascular transmission in the cat. Br. J. Pharmacol. 142, 1171–1181 (2004).
Olesen, J. et al. Calcitonin gene-related peptide (CGRP) receptor antagonist BIBN4096BS is effective in the treatment of migraine attacks. New Eng. J. Med. 350, 1104–1110 (2004). This proof-of-concept study showed that a CGRP antagonist could abort acute migraine.
Petersen, K. A. et al. The novel CGRP-antagonist, BIBN4096BS does not affect the cerebral hemodynamics in healthy volunteers. Cephalalgia 23, 729 (2003).
Sawynok, J. Adenosine receptor activation and nociception. Eur. J. Pharmacol. 347, 1–11 (1998).
Sawynok, J. Purines in pain management. Curr. Opin. Cent. Peripher. Nerv. Syst. Investig. Drugs 1, 27–38 (1999).
Paalzow, G. & Paalzow, L. The effects of caffeine and theophylline on nociceptive stimulation in the rat. Acta Pharmacol. Toxicol. 32, 22–32 (1973).
Sawynok, J., Sweeney, M. I. & White, T. D. Classification of adenosine receptors mediating antinociception in the rat spinal cord. Br. J. Pharmacol. 88, 923–930 (1986).
Sjolund, K.-F., Sollevi, A., Segerdahl, M., Hansson, P. & Lundeberg, T. Intrathecal and systemic R-phenylisopropy-adenosine reduces scratching behaviour in a rat mononeuropathy model. NeuroReport 7, 1856–1860 (1996).
DeLander, G. E. & Hopkins, G. J. Spinal adenosine modulates descending antinociceptive pathways stimulated by morphine. J. Pharmacol. Exp. Therap. 239, 88–93 (1986).
DeLander, G. E. & Hopkins, C. J. Interdependence of spinal adenosinergic, serotonergic and noradrenergic systems mediating antinociception. Neuropharmacology 26, 1791–1794 (1987).
Schindler, M., Harris, C. A., Hayes, B., Papotti, M. & Humphrey, P. P. A. Immunohistochemical localization of adenosine A1 receptors in human brain regions. Neurosci. Lett. 297, 211–215 (2001).
Gurden, M. F. et al. Functional characterisation of three adenosine receptor types. Br. J. Pharmacol. 109, 693–698 (1993).
Sheehan, M. J., Wilson, D. J., Cousins, R. & Giles, H. Relative intrinsic efficacy of adenosine A1 receptor agonists measured using functional and radioligand binding. Br. J. Pharmacol. 131, 34P (2000).
Goadsby, P. J., Hoskin, K. L., Storer, R. J., Edvinsson, L. & Connor, H. E. Adenosine (A1) receptor agonists inhibit trigeminovascular nociceptive transmission. Brain 125, 1392–1401 (2002). This pivotal paper established an adenosine A 1 receptor agonist as a target for acute migraine therapy.
Santicioli, P., Delbianco, E. & Maggi, C. A. Adenosine A1 receptors mediate the presynaptic inhibition of calcitonin gene related peptide release by adenosine in the rat spinal cord. Eur. J. Pharmacol. 231, 139–142 (1993).
Honey, A. C., Bland-Ward, P. A., Connor, H. E., Feniuk, W. & Humphrey, P. P. A. Study of an adenosine A1 receptor agonist on trigeminally evoked dural blood vessel dilation in the anaesthetized rat. Cephalalgia 22, 260–264 (2000).
Kaube, H., Katsarava, Z., Kaufer, T., Diener, H.-C. & Ellrich, J. A new method to increase the nociception specificity of the human blink reflex. Clin. Neurophysiol. 111, 413–416 (2000).
Giffin, N. J. et al. Effect of adenosine A1 receptor agonist GR79236 on trigeminal nociception with blink reflex recordings in healthy human subjects. Cephalalgia 23, 287–292 (2003).
Humphrey, P. P. et al. Inhibition of trigeminal nociceptive afferents by adenosine A1 receptor activation: a novel approach towards the design of new anti-migraine compounds. Cephalalgia 21, 268–269 (2001).
Meunier, J., Mouledous, L. & Topham, C. M. The nociceptin (ORL1) receptor: molecular cloning and functional architecture. Peptides 21, 893–900 (2000).
Reinscheid, R. K., Nothacker, H. & Civelli, O. The orphanin FQ/nociceptin gene: structure, tissue distribution of expression and functional implications obtained from knockout mice. Peptides 21, 901–906 (2000).
Mogil, J. S. & Pasternak, G. W. The molecular and behavioral pharmacology of the orphanin FQ/nociceptin peptide and receptor family. Pharmacol. Rev. 53, 381–415 (2001).
Reinscheid, R. K. et al. Orphanin FQ: a neuropeptide that activates an opioid-like G protein-coupled receptor. Science 270, 792–794 (1995).
Darland, T. & Grandy, D. K. The orphanin FQ system: an emerging target for the management of pain? Br. J. Anaesth. 81, 29–37 (1998).
Hou, M., Tajti, J., Uddman, R. & Edvinsson, L. Demonstration of nociceptin positive cells and opioid-receptor like-1 in human trigeminal ganglion. Cephalalgia 21, 402 (2001).
Williamson, D. J., Hargreaves, R. J., Hill, R. G. & Shepheard, S. L. Intravital microscope studies on the effects of neurokinin agonists and calcitonin gene-related peptide on dural blood vessel diameter in the anaesthetized rat. Cephalalgia 17, 518–524 (1997).
Bartsch, T., Akerman, S. & Goadsby, P. J. The ORL-1 (NOP1) receptor ligand nociceptin/orphanin FQ (N/OFQ) inhibits neurogenic vasodilatation in the rat. Neuropharmacology 43, 991–998 (2002).
Okuda-Ashitaka, E. et al. Nocistatin, a peptide that blocks nociceptin action in pain transmission. Nature 392, 286–289 (1998).
Okuda-Ashitaka, E. & Ito, S. Nocistatin: a novel neuropeptide encoded by the gene for the nociceptin/orphanin FQ precursor. Peptides 21, 1101–1109 (2000).
Caterina, M. J. et al. The capsaicin receptor: a heat-activated ion channel in the pain pathway. Nature 389, 816–824 (1997).
Joo, F., Szolcsanyi, J. & Jancso-Gabor, A. Mitochondrial alterations in the spinal ganglion cells of the rat accompanying the long-lasting sensory disturbance induced by capsaicin. Life Sci. 8, 621–626 (1969).
Guo, A., Vulchanova, L., Wang, J., Li, X. & Elde, R. Immunocytochemical localization of the vanilloid receptor 1 (VR1): relationship to neuropeptides, the P2X3 purinoceptor and IB4 binding sites. Eur. J. Neurosci. 11, 946–958 (1999).
Ichikawa, H. & Sugimoto, T. VR1-immunoreactive primary sensory neurons in the rat trigeminal ganglion. Brain Res. 890, 184–188 (2001).
Hou, M., Uddman, R., Tajti, J., Kanje, M. & Edvinsson, L. Capsaicin receptor immunoreactivity in the human trigeminal ganglion. Neurosci. Lett. 330, 223–226 (2002).
Akerman, S., Kaube, H. & Goadsby, P. J. Vanilloid type 1 receptor (VR1) evoked CGRP release plays a minor role in causing dural vessel dilation via the trigeminovascular system. Br. J. Pharmacol. 140, 718–724 (2003).
Shepheard, S. L., Williamson, D. J., Beer, M. S., Hill, R. G. & Hargreaves, R. J. Differential effects of 5-HT1B/1D receptor agonists on neurogenic dural plasma extravasation and vasodilation in anaesthetized rats. Neuropharmacology 36, 525–533 (1997).
Williamson, D. J., Shepheard, S. L., Hill, R. G. & Hargreaves, R. J. The novel anti-migraine agent rizatriptan inhibits neurogenic dural vasodilation and extravasation. Eur. J. Pharmacol. 328, 61–64 (1997).
Matsuda, L. A., Lolait, S. J., Brownstein, M. J., Young, A. C. & Bonner, T. I. Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature 346, 561–564 (1990).
Hoehe, M. R. et al. Genetic and physical mapping of the human cannabinoid receptor gene to chromosome 6q14-q15. New Biol. 3, 880–885 (1991).
Devane, W. A. et al. Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science 258, 1946–1949 (1992).
Munro, S., Thomas, K. L. & Abu-Shaar, M. Molecular characterization of a peripheral receptor for cannabinoids. Nature 365, 61–65 (1993).
Dewey, W. L. Cannabinoid pharmacology. Pharmacol. Rev. 38, 151–178 (1986).
Smith, P. B. et al. The pharmacological activity of anandamide, a putative endogenous cannabinoid, in mice. J. Pharmacol. Exp. Ther. 270, 219–227 (1994).
Adams, I. B., Compton, D. R. & Martin, B. R. Assessment of anandamide interaction with the cannabinoid brain receptor: SR 141716A antagonism studies in mice and autoradiographic analysis of receptor binding in rat brain. J. Pharmacol. Exp. Ther. 284, 1209–1217 (1998).
Crawley, J. N. et al. Anandamide, an endogenous ligand of the cannabinoid receptor, induces hypomotility and hypothermia in vivo in rodents. Pharmacol. Biochem. Behav. 46, 967–972 (1993).
Akerman, S., Kaube, H. & Goadsby, P. J. Anandamide is able to inhibit trigeminal neurons using an in vivo model of trigeminovascular-mediated nociception. J. Pharmacol. Exp. Ther. 309, 56–63 (2004). This important paper established CB 1 receptor targets in the trigeminovascular system.
Zygmunt, P. M. et al. Vanilloid receptors on sensory nerves mediate the vasodilator action of anandamide. Nature 400, 452–457 (1999).
Akerman, S., Kaube, H. & Goadsby, P. J. Anandamide shows both cannabinoid and vanilloid properties in an in vivo model of trigeminovascular mediated headpain. Cephalalgia 23, 646 (2003).
Sakurai, T. et al. Orexins and orexin receptors: a family of hypothalamic neuropeptides and G protein-coupled receptors that regulate feeding behavior. Cell 92, 696–697 (1998).
de Lecea, L. et al. The hypocretins: hypothalamus-specific peptides with neuroexcitatory activity. Proc. Natl Acad. Sci. USA 95, 322–327 (1998).
Trivedi, P., Yu, H., MacNeil, D. J., Van der Ploeg, L. H. & Guan, X. M. Distribution of orexin receptor mRNA in the rat brain. FEBS Lett. 438, 71–75 (1998).
Peyron, C. et al. Neurons containing hypocretin (orexin) project to multiple neuronal systems. J. Neurosci. 18, 9996–10015 (1998).
Marcus, J. N. et al. Differential expression of orexin receptors 1 and 2 in the rat brain. J. Comp. Neurol. 435, 6–25 (2001).
Date, Y. et al. Orexins, orexigenic hypothalamic peptides, interact with autonomic, neuroendocrine and neuroregulatory systems. Proc. Natl Acad. Sci. USA 96, 748–753 (1999).
Nambu, T. et al. Distribution of orexin neurons in the adult rat brain. Brain Res. 827, 243–260 (1999).
Smart, D. & Jerman, J. The physiology and pharmacology of the orexins. Pharmacol. Ther. 94, 51 (2002). An excellent review on orexins.
van den Pol, A. N., Gao, X. B., Obrietan, K., Kilduff, T. S. & Belousov, A. B. Presynaptic and postsynaptic actions and modulation of neuroendocrine neurons by a new hypothalamic peptide, hypocretin/orexin. J. Neurosci. 18, 7962–7971 (1998).
Siegel, J. M. Narcolepsy: a key role for hypocretins (orexins). Cell 98, 409–412 (1999).
Bingham, S. et al. Orexin-A, an hypothalamic peptide with analgesic properties. Pain 92, 81–90 (2001).
Yamamoto, T., Nozaki-Taguchi, N. & Chiba, T. Analgesic effect of intrathecally administered orexin-A in the rat formalin test and in the rat hot plate test. Br. J. Pharmacol. 137, 170–176 (2002).
Grudt, T. J., van den Pol, A. N. & Perl, E. R. Hypocretin-2 (orexin-B) modulation of superficial dorsal horn activity in rat. J. Physiol. 538, 517–525 (2002).
Benjamin, L. et al. Hypothalamic activation after stimulation of the superior sagittal sinus in the cat: a Fos study. Neurobiol. Dis. 16, 500–505 (2004).
Bartsch, T., Levy, M. J., Knight, Y. E. & Goadsby, P. J. Differential modulation of nociceptive dural input to [hypocretin] orexin A and B receptor activation in the posterior hypothalamic area. Pain 109, 367–378 (2004). This interesting paper showed the differential effects of orexin A and B in the hypothalamus.
Hagan, J. J. et al. Orexin A activates locus coeruleus cell firing and increases arousal in the rat. Proc. Natl Acad. Sci. USA 96, 10911–10916 (1999).
Soffin, E. M. et al. SB-334867-A antagonises orexin mediated excitation in the locus coeruleus. Neuropharmacology 42, 127–133 (2002).
Thomsen, L. L. & Olesen, J. Nitric oxide in primary headaches. Curr. Opin. Neurol. 14, 315–321 (2001).
Thomsen, L. L. & Olesen, J. A pivotal role of nitric oxide in migraine pain. Ann. NY Acad. Sci. 835, 363–372 (1997). An excellent review of NO mechanisms in migraine.
Olesen, J., Thomsen, L. L., Lassen, L. H. & Olesen, I. J. The nitric oxide hypothesis of migraine and other vascular headaches. Cephalalgia 15, 94–100 (1995).
Iversen, H. K., Olesen, J. & Tfelt-Hansen, P. Intravenous nitroglycerin as an experimental headache model. Basic characteristics. Pain 38, 17–24 (1989).
Giffin, N. J. et al. Premonitory symptoms in migraine: an electronic diary study. Neurology 60, 935–940 (2003).
Kruuse, C., Thomsen, L. L., Birk, S. & Olesen, J. Migraine can be induced by sildenafil without changes in middle cerebral artery diameter. Brain 126, 241–247 (2003).
Reuter, U. et al. Delayed inflammation in rat meninges: implications for migraine pathophysiology. Brain 124, 2490–2502 (2001).
Hoskin, K. L., Bulmer, D. C. E. & Goadsby, P. J. Fos expression in the trigeminocervical complex of the cat after stimulation of the superior sagittal sinus is reduced by L-NAME. Neurosci. Lett. 266, 173–176 (1999).
Lipton, R. B., Diamond, S., Reed, M., Diamond, M. L. & Stewart, W. F. Migraine diagnosis and treatment: results from the American Migraine Study II. Headache 41, 638–645 (2001).
Matharu, M. S. et al. Central neuromodulation in chronic migraine patients with suboccipital stimulators: a PET study. Brain 127, 220–230 (2004).
Acknowledgements
The work of the author is supported by the Wellcome Trust.
Author information
Authors and Affiliations
Ethics declarations
Competing interests
P.J.G. is a consultant for or has done research with GSK, Pfizer, Astra Zeneca, Allergen, Medtronic, BMS and Boehringer.
Related links
Related links
DATABASES
Entrez Gene
OMIM
Glossary
- HABITUATION
-
A reduced response to the same sensory input.
- CONTINGENT NEGATIVE VARIATION
-
A negative wave that is associated with an anticipatory stimulus.
- CORTICAL SPREADING DEPRESSION
-
A wave of neuronal activation followed by inhibition that moves across the cortex at a characteristically slow rate of 3–6 mm per min.
- TRIGEMINAL BLINK REFLEX
-
The response of the muscles around the eye to an electrical stimulus that causes them to close (blink), which can be measured using recording electrodes.
- INTRAVITAL MODEL OF WILLIAMS AND HARGREAVES
-
An experimental animal system in which vessels in the rat dura mater can be directly studied by measuring their diameter in response to stimuli.
- ALLODYNIA
-
Pain from non-noxious heat, cold or pressure.
Rights and permissions
About this article
Cite this article
Goadsby, P. Can we Develop Neurally Acting Drugs for the Treatment of Migraine?. Nat Rev Drug Discov 4, 741–750 (2005). https://doi.org/10.1038/nrd1822
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrd1822
This article is cited by
-
Dynamic Interactions Between Plasma IL-1 Family Cytokines and Central Endogenous Opioid Neurotransmitter Function in Humans
Neuropsychopharmacology (2015)
-
Excitatory Neurotransmitters in Brain Regions in Interictal Migraine Patients
Molecular Pain (2009)
-
CGRP receptor antagonist meets Phase III migraine end points
Nature Reviews Drug Discovery (2009)
-
Pain perception and laser evoked potentials during menstrual cycle in migraine
The Journal of Headache and Pain (2009)
-
The effects of the TRPV1 receptor antagonist SB-705498 on trigeminovascular sensitisation and neurotransmission
Naunyn-Schmiedeberg's Archives of Pharmacology (2009)