Abstract
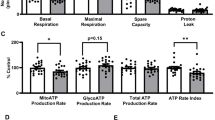
Alterations of mitochondrial and glycolytic energy pathways related to aging could contribute to cerebrovascular dysfunction. We studied the impact of aging on energetics of primary human brain microvascular endothelial cells (HBMECs) by comparing the young (passages 7–9), pre-senescent (passages 13–15), and senescent (passages 20–21) cells. Pre-senescent HBMECs displayed decreased telomere length and undetectable telomerase activity although markers of senescence were unaffected. Bioenergetics in HBMECs were determined by measuring the oxygen consumption (OCR) and extracellular acidification (ECAR) rates. Cellular ATP production in young HBMECs was predominantly dependent on glycolysis with glutamine as the preferred fuel for mitochondrial oxidative phosphorylation (OXPHOS). In contrast, pre-senescent HBMECs displayed equal contribution to ATP production rate from glycolysis and OXPHOS with equal utilization of glutamine, glucose, and fatty acids as mitofuels. Compared to young, pre-senescent HBMECs showed a lower overall ATP production rate that was characterized by diminished contribution from glycolysis. Impairments of glycolysis displayed by pre-senescent cells included reduced basal glycolysis, compensatory glycolysis, and non-glycolytic acidification. Furthermore, impairments of mitochondrial respiration in pre-senescent cells involved the reduction of maximal respiration and spare respiratory capacity but intact basal and ATP production-related OCR. Proton leak and non-mitochondrial respiration, however, were unchanged in the pre-senescent HBMECs. HBMECS at passages 20–21 displayed expression of senescence markers and continued similar defects in glycolysis and worsened OXPHOS. Thus, for the first time, we characterized the bioenergetics of pre-senescent HBMECs comprehensively to identify the alterations of the energy pathways that could contribute to aging.







Similar content being viewed by others
References
Erdő F, Denes L and de Lange E. Age-associated physiological and pathological changes at the blood-brain barrier: A review. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism 2017; 37: 4–24. 2016/11/12. https://doi.org/10.1177/0271678x16679420.
Toth P, Tarantini S, Csiszar A and Ungvari Z. Functional vascular contributions to cognitive impairment and dementia: mechanisms and consequences of cerebral autoregulatory dysfunction, endothelial impairment, and neurovascular uncoupling in aging. American journal of physiology Heart and circulatory physiology 2017; 312: H1-h20. 2016/10/30. https://doi.org/10.1152/ajpheart.00581.2016.
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O'Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, VanWagner LB, Wilkins JT, Wong SS, Virani SS, American Heart Association Council on E, Prevention Statistics C and Stroke Statistics S. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation 2019; 139: e56-e528. 2019/02/01. https://doi.org/10.1161/CIR.0000000000000659.
Eelen G, de Zeeuw P, Simons M and Carmeliet P. Endothelial cell metabolism in normal and diseased vasculature. Circulation research 2015; 116: 1231–1244. 2015/03/31. https://doi.org/10.1161/circresaha.116.302855.
Eelen G, Cruys B, Welti J, De Bock K and Carmeliet P. Control of vessel sprouting by genetic and metabolic determinants. Trends Endocrinol Metab 2013; 24: 589–596. 2013/10/01. https://doi.org/10.1016/j.tem.2013.08.006.
Eelen G, de Zeeuw P, Treps L, Harjes U, Wong BW and Carmeliet P. Endothelial Cell Metabolism. Physiol Rev 2018; 98: 3–58. 2017/11/24. https://doi.org/10.1152/physrev.00001.2017.
Caja S and Enríquez JA. Mitochondria in endothelial cells: Sensors and integrators of environmental cues. Redox biology 2017; 12: 821–827. 2017/04/28. https://doi.org/10.1016/j.redox.2017.04.021.
Oldendorf WH, Cornford ME and Brown WJ. The large apparent work capability of the blood-brain barrier: a study of the mitochondrial content of capillary endothelial cells in brain and other tissues of the rat. Ann Neurol 1977; 1: 409–417. 1977/05/01. https://doi.org/10.1002/ana.410010502.
Doll DN, Hu H, Sun J, Lewis SE, Simpkins JW and Ren X. Mitochondrial crisis in cerebrovascular endothelial cells opens the blood-brain barrier. Stroke 2015; 46: 1681–1689. 2015/04/30. https://doi.org/10.1161/strokeaha.115.009099.
Diebold LP, Gil HJ, Gao P, Martinez CA, Weinberg SE and Chandel NS. Mitochondrial complex III is necessary for endothelial cell proliferation during angiogenesis. Nature metabolism 2019; 1: 158–171. 2019/05/21. https://doi.org/10.1038/s42255-018-0011-x.
De Bock K, Georgiadou M, Schoors S, Kuchnio A, Wong BW, Cantelmo AR, Quaegebeur A, Ghesquiere B, Cauwenberghs S, Eelen G, Phng LK, Betz I, Tembuyser B, Brepoels K, Welti J, Geudens I, Segura I, Cruys B, Bifari F, Decimo I, Blanco R, Wyns S, Vangindertael J, Rocha S, Collins RT, Munck S, Daelemans D, Imamura H, Devlieger R, Rider M, Van Veldhoven PP, Schuit F, Bartrons R, Hofkens J, Fraisl P, Telang S, Deberardinis RJ, Schoonjans L, Vinckier S, Chesney J, Gerhardt H, Dewerchin M and Carmeliet P. Role of PFKFB3-driven glycolysis in vessel sprouting. Cell 2013; 154: 651–663. 2013/08/06. https://doi.org/10.1016/j.cell.2013.06.037.
Salmina AB, Kuvacheva NV, Morgun AV, Komleva YK, Pozhilenkova EA, Lopatina OL, Gorina YV, Taranushenko TE and Petrova LL. Glycolysis-mediated control of blood-brain barrier development and function. The international journal of biochemistry & cell biology 2015; 64: 174–184. 2015/04/23. https://doi.org/10.1016/j.biocel.2015.04.005.
Kuosmanen SM, Sihvola V, Kansanen E, Kaikkonen MU and Levonen AL. MicroRNAs mediate the senescence-associated decline of NRF2 in endothelial cells. Redox biology 2018; 18: 77–83. 2018/07/10. https://doi.org/10.1016/j.redox.2018.06.007.
Sure VN, Sakamuri S, Sperling JA, Evans WR, Merdzo I, Mostany R, Murfee WL, Busija DW and Katakam PVG. A novel high-throughput assay for respiration in isolated brain microvessels reveals impaired mitochondrial function in the aged mice. Geroscience 2018; 40: 365–375. 2018/08/04. https://doi.org/10.1007/s11357-018-0037-8.
Xu Y, An X, Guo X, Habtetsion TG, Wang Y, Xu X, Kandala S, Li Q, Li H, Zhang C, Caldwell RB, Fulton DJ, Su Y, Hoda MN, Zhou G, Wu C and Huo Y. Endothelial PFKFB3 plays a critical role in angiogenesis. Arterioscler Thromb Vasc Biol 2014; 34: 1231–1239. 2014/04/05. https://doi.org/10.1161/ATVBAHA.113.303041.
Unterluggauer H, Mazurek S, Lener B, Hutter E, Eigenbrodt E, Zwerschke W and Jansen-Durr P. Premature senescence of human endothelial cells induced by inhibition of glutaminase. Biogerontology 2008; 9: 247–259. 2008/03/05. https://doi.org/10.1007/s10522-008-9134-x.
Yetkin-Arik B, Vogels IMC, Neyazi N, van Duinen V, Houtkooper RH, van Noorden CJF, Klaassen I and Schlingemann RO. Endothelial tip cells in vitro are less glycolytic and have a more flexible response to metabolic stress than non-tip cells. Scientific reports 2019; 9: 10414. 2019/07/20. https://doi.org/10.1038/s41598-019-46503-2.
Xing CY, Tarumi T, Liu J, Zhang Y, Turner M, Riley J, Tinajero CD, Yuan LJ and Zhang R. Distribution of cardiac output to the brain across the adult lifespan. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism 2017; 37: 2848–2856. 2016/11/01. https://doi.org/10.1177/0271678X16676826.
He X, Zeng H, Chen ST, Roman RJ, Aschner JL, Didion S and Chen JX. Endothelial specific SIRT3 deletion impairs glycolysis and angiogenesis and causes diastolic dysfunction. J Mol Cell Cardiol 2017; 112: 104–113. 2017/09/25. https://doi.org/10.1016/j.yjmcc.2017.09.007.
Graves SI and Baker DJ. Implicating endothelial cell senescence to dysfunction in the ageing and diseased brain. Basic Clin Pharmacol Toxicol 2020; 127: 102–110. 2020/03/13. https://doi.org/10.1111/bcpt.13403.
Yepuri G, Sukhovershin R, Nazari-Shafti TZ, Petrascheck M, Ghebre YT and Cooke JP. Proton Pump Inhibitors Accelerate Endothelial Senescence. Circulation research 2016; 118: e36–42. 2016/05/12. https://doi.org/10.1161/circresaha.116.308807.
Yetkin-Arik B, Vogels IMC, Nowak-Sliwinska P, Weiss A, Houtkooper RH, Van Noorden CJF, Klaassen I and Schlingemann RO. The role of glycolysis and mitochondrial respiration in the formation and functioning of endothelial tip cells during angiogenesis. Scientific reports 2019; 9: 12608. 2019/09/01. https://doi.org/10.1038/s41598-019-48676-2.
Otolorin EO, Falase EA and Ladipo OA. A comparative study of three oral contraceptives in Ibadan: Norinyl 1/35, Lo-Ovral and Noriday 1/50. African journal of medicine and medical sciences 1990; 19: 15–22. 1990/03/01.
Lee MJ, Jang Y, Han J, Kim SJ, Ju X, Lee YL, Cui J, Zhu J, Ryu MJ, Choi SY, Chung W, Heo C, Yi HS, Kim HJ, Huh YH, Chung SK, Shong M, Kweon GR and Heo JY. Endothelial-specific Crif1 deletion induces BBB maturation and disruption via the alteration of actin dynamics by impaired mitochondrial respiration. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism 2020; 40: 1546–1561. 2020/01/29. https://doi.org/10.1177/0271678x19900030.
Desler C, Hansen TL, Frederiksen JB, Marcker ML, Singh KK and Juel Rasmussen L. Is There a Link between Mitochondrial Reserve Respiratory Capacity and Aging? Journal of aging research 2012; 2012: 192503. 2012/06/22. https://doi.org/10.1155/2012/192503.
Bell SM, De Marco M, Barnes K, Shaw PJ, Ferraiuolo L, Blackburn DJ, Mortiboys H and Venneri A. Deficits in Mitochondrial Spare Respiratory Capacity Contribute to the Neuropsychological Changes of Alzheimer's Disease. Journal of personalized medicine 2020; 10 2020/05/06. https://doi.org/10.3390/jpm10020032.
Brown WR and Thore CR. Review: cerebral microvascular pathology in ageing and neurodegeneration. Neuropathology and applied neurobiology 2011; 37: 56–74. 2010/10/16. https://doi.org/10.1111/j.1365-2990.2010.01139.x.
Goodall EF, Wang C, Simpson JE, Baker DJ, Drew DR, Heath PR, Saffrey MJ, Romero IA, Wharton SB. Age-associated changes in the blood-brain barrier: comparative studies in human and mouse. Neuropathology Applied Neurobiology. 2018;44:328–40. https://doi.org/10.1111/nan.12408.
Stefanatos R, Sanz A. The role of mitochondrial ROS in the aging brain. FEBS Letters. 2018;592:743–58. https://doi.org/10.1002/1873-3468.12902.
Wilkins HM, Swerdlow RH. Mitochondrial links between brain aging and Alzheimer’s disease. Translational Neurodegeneration. 2021;10:33. https://doi.org/10.1186/s40035-021-00261-2.
Presa JL, Saravia F, Bagi Z and Filosa JA. Vasculo-Neuronal Coupling and Neurovascular Coupling at the Neurovascular Unit: Impact of Hypertension. Frontiers in Physiology 2020; 11. Review. https://doi.org/10.3389/fphys.2020.584135.
Longden TA, Dabertrand F, Koide M, Gonzales AL, Tykocki NR, Brayden JE, Hill-Eubanks D, Nelson MT. Capillary K+-sensing initiates retrograde hyperpolarization to increase local cerebral blood flow. Nature Neuroscience. 2017;20:717–26. https://doi.org/10.1038/nn.4533.
Eelen G. Zeeuw Pd, Treps L, Harjes U, Wong BW and Carmeliet P. Endothelial Cell Metabolism Physiological Reviews. 2018;98:3–58. https://doi.org/10.1152/physrev.00001.2017.
Schoors S, Bruning U, Missiaen R, Queiroz KC, Borgers G, Elia I, Zecchin A, Cantelmo AR, Christen S, Goveia J, Heggermont W, Goddé L, Vinckier S, Van Veldhoven PP, Eelen G, Schoonjans L, Gerhardt H, Dewerchin M, Baes M, De Bock K, Ghesquière B, Lunt SY, Fendt SM and Carmeliet P. Fatty acid carbon is essential for dNTP synthesis in endothelial cells. Nature 2015; 520: 192–197. 2015/04/02. https://doi.org/10.1038/nature14362.
Huang H, Vandekeere S, Kalucka J, Bierhansl L, Zecchin A, Brüning U, Visnagri A, Yuldasheva N, Goveia J, Cruys B, Brepoels K, Wyns S, Rayport S, Ghesquière B, Vinckier S, Schoonjans L, Cubbon R, Dewerchin M, Eelen G and Carmeliet P. Role of glutamine and interlinked asparagine metabolism in vessel formation. Embo j 2017; 36: 2334–2352. 2017/07/01. https://doi.org/10.15252/embj.201695518.
Quijano C, Cao L, Fergusson MM, Romero H, Liu J, Gutkind S, Rovira, II, Mohney RP, Karoly ED and Finkel T. Oncogene-induced senescence results in marked metabolic and bioenergetic alterations. Cell cycle (Georgetown, Tex) 2012; 11: 1383–1392. 2012/03/17. https://doi.org/10.4161/cc.19800.
Fafián-Labora J, Carpintero-Fernández P, Jordan SJD, Shikh-Bahaei T, Abdullah SM, Mahenthiran M, Rodríguez-Navarro JA, Niklison-Chirou MV and O'Loghlen A. FASN activity is important for the initial stages of the induction of senescence. Cell death & disease 2019; 10: 318. 2019/04/10. https://doi.org/10.1038/s41419-019-1550-0.
Liu Y, Bloom SI and Donato AJ. The role of senescence, telomere dysfunction and shelterin in vascular aging. Microcirculation 2019; 26: e12487. 2018/06/21. https://doi.org/10.1111/micc.12487.
Tarantini S, Yabluchanskiy A, Csipo T, Fulop G, Kiss T, Balasubramanian P, DelFavero J, Ahire C, Ungvari A, Nyul-Toth A, Farkas E, Benyo Z, Toth A, Csiszar A and Ungvari Z. Treatment with the poly(ADP-ribose) polymerase inhibitor PJ-34 improves cerebromicrovascular endothelial function, neurovascular coupling responses and cognitive performance in aged mice, supporting the NAD+ depletion hypothesis of neurovascular aging. Geroscience 2019; 41: 533–542. 2019/11/05. https://doi.org/10.1007/s11357-019-00101-2.
Wardi L, Alaaeddine N, Raad I, Sarkis R, Serhal R, Khalil C, Hilal G. Glucose restriction decreases telomerase activity and enhances its inhibitor response on breast cancer cells: possible extra-telomerase role of BIBR 1532. Cancer Cell International. 2014;14(60):20140704. https://doi.org/10.1186/1475-2867-14-60.
Roh J-i, Kim Y, Oh J, Kim Y, Lee J, Lee J, Chun K-H and Lee H-W. Hexokinase 2 is a molecular bridge linking telomerase and autophagy. PLOS ONE 2018; 13: e0193182. https://doi.org/10.1371/journal.pone.0193182.
Zheng Q, Huang J and Wang G. Mitochondria, Telomeres and Telomerase Subunits. Frontiers in Cell and Developmental Biology 2019; 7. Review. https://doi.org/10.3389/fcell.2019.00274.
Passos JF, Saretzki G, Ahmed S, Nelson G, Richter T, Peters H, Wappler I, Birket MJ, Harold G, Schaeuble K, Birch-Machin MA, Kirkwood TBL, von Zglinicki T. Mitochondrial Dysfunction Accounts for the Stochastic Heterogeneity in Telomere-Dependent Senescence. PLoS Biology. 2007;5: e110. https://doi.org/10.1371/journal.pbio.0050110.
Stanhewicz AE, Wenner MM and Stachenfeld NS. Sex differences in endothelial function important to vascular health and overall cardiovascular disease risk across the lifespan. American journal of physiology Heart and circulatory physiology 2018; 315: H1569-h1588. 20180914. https://doi.org/10.1152/ajpheart.00396.2018.
Yao CH, Liu GY, Wang R, Moon SH, Gross RW and Patti GJ. Identifying off-target effects of etomoxir reveals that carnitine palmitoyltransferase I is essential for cancer cell proliferation independent of β-oxidation. PLoS biology 2018; 16: e2003782. 2018/03/30. https://doi.org/10.1371/journal.pbio.2003782.
Xu FY, Taylor WA, Hurd JA, Hatch GM. Etomoxir mediates differential metabolic channeling of fatty acid and glycerol precursors into cardiolipin in H9c2 cells. Journal of Lipid Research. 2003;44:415–23. https://doi.org/10.1194/jlr.M200335-JLR200.
Zhong Y, Li X, Yu D, Li X, Li Y, Long Y, Yuan Y, Ji Z, Zhang M, Wen JG, Nesland JM and Suo Z. Application of mitochondrial pyruvate carrier blocker UK5099 creates metabolic reprogram and greater stem-like properties in LnCap prostate cancer cells in vitro. Oncotarget 2015; 6: 37758–37769. 2015/09/29. https://doi.org/10.18632/oncotarget.5386.
Wang J, Cui Y, Yu Z, Wang W, Cheng X, Ji W, Guo S, Zhou Q, Wu N, Chen Y, Chen Y, Song X, Jiang H, Wang Y, Lan Y, Zhou B, Mao L, Li J, Yang H, Guo W, Yang X. Brain Endothelial Cells Maintain Lactate Homeostasis and Control Adult Hippocampal Neurogenesis. Cell Stem Cell. 2019;25:754-767.e759. https://doi.org/10.1016/j.stem.2019.09.009.
Gray LR, Tompkins SC and Taylor EB. Regulation of pyruvate metabolism and human disease. Cell Mol Life Sci 2014; 71: 2577–2604. 12/21. https://doi.org/10.1007/s00018-013-1539-2.
Robinson MM, McBryant SJ, Tsukamoto T, Rojas C, Ferraris DV, Hamilton SK, Hansen JC and Curthoys NP. Novel mechanism of inhibition of rat kidney-type glutaminase by bis-2-(5-phenylacetamido-1,2,4-thiadiazol-2-yl)ethyl sulfide (BPTES). The Biochemical journal 2007; 406: 407–414. 2007/06/22. https://doi.org/10.1042/bj20070039.
Acknowledgements
We thank Ms. Sufen Zheng for her technical help with the studies.
Funding
This research project was supported by the National Institutes of Health: National Institute of Neurological Disorders and Stroke (NS094834 and NS114286—P.V. Katakam; NS114286 – R. Mostany; NS099539 – X. Wang), National Institute on Aging (AG047296 – R. Mostany; AG-063345 – D. Busija; AG074489 – P.V. Katakam and R. Mostany), National Heart, Lung, Blood Institute (HL093554 – D. Busija; HL133619 – S. Lindsey), and National Institute of General Medical Sciences (NS094834—P.V. Katakam). In addition, the study was supported by American Heart Association (National Center Scientist Development Grant, 14SDG20490359—P.V. Katakam; Greater Southeast Affiliate Predoctoral Fellowship Award, 16PRE27790122—V.N. Sure; Predoctoral Fellowship Award, 20PRE35211153—W.R. Evans. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Sakamuri, S.S.V.P., Sure, V.N., Kolli, L. et al. Glycolytic and Oxidative Phosphorylation Defects Precede the Development of Senescence in Primary Human Brain Microvascular Endothelial Cells. GeroScience 44, 1975–1994 (2022). https://doi.org/10.1007/s11357-022-00550-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11357-022-00550-2