Abstract
Purpose of Review
Hereditary sensory and autonomic neuropathies (HSANs) are a clinically heterogeneous group of inherited neuropathies featuring prominent sensory and autonomic involvement. Classification of HSAN is based on mode of inheritance, genetic mutation, and phenotype. In this review, we discuss the recent additions to this classification and the important updates on management with a special focus on the recently investigated disease-modifying agents.
Recent Findings
In this past decade, three more HSAN types were added to the classification creating even more diversity in the genotype–phenotype. Clinical trials are underway for disease-modifying and symptomatic therapeutics, targeting mainly HSAN type III.
Summary
Obtaining genetic testing leads to accurate diagnosis and guides focused management in the setting of such a diverse and continuously growing phenotype. It also increases the wealth of knowledge on HSAN pathophysiologies which paves the way toward development of targeted genetic treatments in the era of precision medicine.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Nelaton M. Affection singuliere des os du pied. Gaz Hop Civ Milit 1852;4:13–12.
Ota M, Ellefson RD, Lambert EH, Dyck PJ. Hereditary sensory neuropathy, type II. Clinical, electrophysiologic, histologic, and biochemical studies of a Quebec kinship. Arch Neurol. 1973;29:23–37.
Dyck PJ. Neuronal atrophy and degeneration predominantly affecting peripheral sensory and autonomic neurons. In: Dyck PJ, Thomas PK, Griffin JW, Low PA, Poduslo JF, editors. Peripheral neuropathy. 3rd ed. Philadelphia: WB Saunders Co; 1993. p. 1065–93.
Verhoeven K, Timmerman V, Mauko B, Pieber TR, De Jonghe P, Auer-Grumbach M. Recent advances in hereditary sensory and autonomic neuropathies. Curr Opin Neurol. 2006;19:474–80. https://doi.org/10.1097/01.wco.0000245370.82317.f6.
Houlden H, Blake J, Reilly MM. Hereditary sensory neuropathies. Curr Opin Neurol. 2004;17:569–77.
Nicholson GA, Dawkins JL, Blair IP, Kennerson ML, Gordon MJ, Cherryson AK, et al. The gene for hereditary sensory neuropathy type I (HSN-I) maps to chromosome 9q22.1-q22.3. Nat Genet. 1996;13:101–4. https://doi.org/10.1038/ng0596-101.
Denny-Brown D. Hereditary sensory radicular neuropathy. J Neurol Neurosurg Psychiatry. 1951;14:237–52.
Leplat M, editor. Dictionnaire de medecine en 30 volumes 1846; Paris.
Nelaton M, editor. Affection singuliere des os du pied. Gazette des Hopitaux Civils et Militaires 1852; Paris.
Bejaoui K, Uchida Y, Yasuda S, Ho M, Nishijima M, Brown RH Jr, et al. Hereditary sensory neuropathy type 1 mutations confer dominant negative effects on serine palmitoyltransferase, critical for sphingolipid synthesis. J Clin Invest. 2002;110:1301–8. https://doi.org/10.1172/JCI16450.
Ho KW, Jerath NU. V144D mutation of SPTLC1 can present with both painful and painless phenotypes in hereditary sensory and autonomic neuropathies type I. Case Reports in Genetics. 2018;2018:1898151. https://doi.org/10.1155/2018/1898151.
Houlden H, King R, Blake J, Groves M, Love S, Woodward C, et al. Clinical, pathological and genetic characterization of hereditary sensory and autonomic neuropathy type 1 (HSAN I). Brain. 2006;129:411–25. https://doi.org/10.1093/brain/awh712.
Rotthier A, Auer-Grumbach M, Janssens K, Baets J, Penno A, Almeida-Souza L, et al. Mutations in the SPTLC2 subunit of serine palmitoyltransferase cause hereditary sensory and autonomic neuropathy type I. Am J Hum Genet. 2010;87:513–22. https://doi.org/10.1016/j.ajhg.2010.09.010.
Spring PJ, Kok C, Nicholson GA, Ing AJ, Spies JM, Bassett ML, et al. Autosomal dominant hereditary sensory neuropathy with chronic cough and gastro-oesophageal reflux: clinical features in two families linked to chromosome 3p22-p24. Brain. 2005;128:2797–810. https://doi.org/10.1093/brain/awh653.
Guelly C, Zhu PP, Leonardis L, Papic L, Zidar J, Schabhuttl M, et al. Targeted high-throughput sequencing identifies mutations in atlastin-1 as a cause of hereditary sensory neuropathy type I. Am J Hum Genet. 2011;88:99–105. https://doi.org/10.1016/j.ajhg.2010.12.003.
Kornak U, Mademan I, Schinke M, Voigt M, Krawitz P, Hecht J, et al. Sensory neuropathy with bone destruction due to a mutation in the membrane-shaping atlastin GTPase 3. Brain. 2014;137:683–92. https://doi.org/10.1093/brain/awt357.
Zheng W, Yan Z, He R, Huang Y, Lin A, Huang W, et al. Identification of a novel DNMT1 mutation in a Chinese patient with hereditary sensory and autonomic neuropathy type IE. BMC Neurol. 2018;18:174. https://doi.org/10.1186/s12883-018-1177-2.
Klein CJ, Botuyan MV, Wu Y, Ward CJ, Nicholson GA, Hammans S, et al. Mutations in DNMT1 cause hereditary sensory neuropathy with dementia and hearing loss. Nat Genet. 2011;43:595–600. https://doi.org/10.1038/ng.830.
Axelrod FB. Hereditary sensory and autonomic neuropathies. Familial dysautonomia and other HSANs. Clin Auton Res. 2002;12(Suppl 1):I2–14.
Axelrod FB, Gold-von Simson G. Hereditary sensory and autonomic neuropathies: types II, III, and IV. Orphanet J Rare Dis. 2007;2:39. https://doi.org/10.1186/1750-1172-2-39.
Shekarabi M, Girard N, Riviere JB, Dion P, Houle M, Toulouse A, et al. Mutations in the nervous system—specific HSN2 exon of WNK1 cause hereditary sensory neuropathy type II. J Clin Invest. 2008;118:2496–505. https://doi.org/10.1172/JCI34088.
Wakil SM, Monies D, Hagos S, Al-Ajlan F, Finsterer J, Al Qahtani A, et al. Exome sequencing: mutilating sensory neuropathy with spastic paraplegia due to a mutation in FAM134B gene. Case Reports in Genetics. 2018;2018:9468049. https://doi.org/10.1155/2018/9468049.
Erlich Y, Edvardson S, Hodges E, Zenvirt S, Thekkat P, Shaag A, et al. Exome sequencing and disease-network analysis of a single family implicate a mutation in KIF1A in hereditary spastic paraparesis. Genome Res. 2011;21:658–64. https://doi.org/10.1101/gr.117143.110.
Yuan J, Matsuura E, Higuchi Y, Hashiguchi A, Nakamura T, Nozuma S, et al. Hereditary sensory and autonomic neuropathy type IID caused by an SCN9A mutation. Neurology. 2013;80:1641–9. https://doi.org/10.1212/WNL.0b013e3182904fdd.
Riley CM, Day RL, et al. Central autonomic dysfunction with defective lacrimation; report of five cases. Pediatrics. 1949;3:468–78.
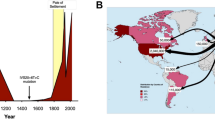
Slaugenhaupt SA, Blumenfeld A, Gill SP, Leyne M, Mull J, Cuajungco MP, et al. Tissue-specific expression of a splicing mutation in the IKBKAP gene causes familial dysautonomia. Am J Hum Genet. 2001;68:598–605.
Carmi S, Hui KY, Kochav E, Liu X, Xue J, Grady F, et al. Sequencing an Ashkenazi reference panel supports population-targeted personal genomics and illuminates Jewish and European origins. Nat Commun. 2014;5:4835. https://doi.org/10.1038/ncomms5835.
Maayan C, Kaplan E, Shachar S, Peleg O, Godfrey S. Incidence of familial dysautonomia in Israel 1977–1981. Clin Genet. 1987;32:106–8.
Close P, Hawkes N, Cornez I, Creppe C, Lambert CA, Rogister B, et al. Transcription impairment and cell migration defects in elongator-depleted cells: implication for familial dysautonomia. Mol Cell. 2006;22:521–31. https://doi.org/10.1016/j.molcel.2006.04.017.
Creppe C, Malinouskaya L, Volvert ML, Gillard M, Close P, Malaise O, et al. Elongator controls the migration and differentiation of cortical neurons through acetylation of alpha-tubulin. Cell. 2009;136:551–64. https://doi.org/10.1016/j.cell.2008.11.043.
Anderson SL, Coli R, Daly IW, Kichula EA, Rork MJ, Volpi SA, et al. Familial dysautonomia is caused by mutations of the IKAP gene. Am J Hum Genet. 2001;68:753–8. https://doi.org/10.1086/318808.
Norcliffe-Kaufmann L, Slaugenhaupt SA, Kaufmann H. Familial dysautonomia: history, genotype, phenotype and translational research. Prog Neurobiol. 2017;152:131–48. https://doi.org/10.1016/j.pneurobio.2016.06.003.
Dong J, Edelmann L, Bajwa AM, Kornreich R, Desnick RJ. Familial dysautonomia: detection of the IKBKAP IVS20(+6T → C) and R696P mutations and frequencies among Ashkenazi Jews. Am J Med Genet. 2002;110:253–7. https://doi.org/10.1002/ajmg.10450.
Lehavi O, Aizenstein O, Bercovich D, Pavzner D, Shomrat R, Orr-Urtreger A, et al. Screening for familial dysautonomia in Israel: evidence for higher carrier rate among Polish Ashkenazi Jews. Genet Test. 2003;7:139–42. https://doi.org/10.1089/109065703322146830.
Dyck PJ, Kawamura Y, Low PA, Shimono M, Solovy JS. The number and sizes of reconstructed peripheral autonomic, sensory and motor neurons in a case or dysautonomia. J Neuropathol Exp Neurol. 1978;37:741–55.
Axelrod FB, Iyer K, Fish I, Pearson J, Sein ME, Spielholz N. Progressive sensory loss in familial dysautonomia. Pediatrics. 1981;67:517–22.
Pearson J, Pytel BA. Quantitative studies of sympathetic ganglia and spinal cord intermedio-lateral gray columns in familial dysautonomia. J Neurol Sci. 1978;39:47–59.
Pearson J, Brandeis L, Goldstein M. Tyrosine hydroxylase immunoreactivity in familial dysautonomia. Science. 1979;206:71–2.
Bickel A, Axelrod FB, Schmelz M, Marthol H, Hilz MJ. Dermal microdialysis provides evidence for hypersensitivity to noradrenaline in patients with familial dysautonomia. J Neurol Neurosurg Psychiatry. 2002;73:299–302.
Goldstein DS, Eldadah B, Sharabi Y, Axelrod FB. Cardiac sympathetic hypo-innervation in familial dysautonomia. Clin Auton Res. 2008;18:115–9. https://doi.org/10.1007/s10286-008-0464-1.
Pearson J, Pytel B. Quantitative studies of ciliary and sphenopalatine ganglia in familial dysautonomia. J Neurol Sci. 1978;39:123–30.
Goadsby PJ. Sphenopalatine ganglion stimulation increases regional cerebral blood flow independent of glucose utilization in the cat. Brain Res. 1990;506:145–8.
Axelrod FB, Hilz MJ, Berlin D, Yau PL, Javier D, Sweat V, et al. Neuroimaging supports central pathology in familial dysautonomia. J Neurol. 2010;257:198–206. https://doi.org/10.1007/s00415-009-5293-1.
Axelrod FB. Familial dysautonomia. Muscle Nerve. 2004;29:352–63. https://doi.org/10.1002/mus.10499.
Bernardi L, Hilz M, Stemper B, Passino C, Welsch G, Axelrod FB. Respiratory and cerebrovascular responses to hypoxia and hypercapnia in familial dysautonomia. Am J Respir Crit Care Med. 2003;167:141–9. https://doi.org/10.1164/rccm.200207-677OC.
Axelrod FB, Nachtigal R, Dancis J. Familial dysautonomia: diagnosis, pathogenesis and management. Adv Pediatr Infect Dis. 1974;21:75–96.
Hilz MJ, Stemper B, Axelrod FB. Sympathetic skin response differentiates hereditary sensory autonomic neuropathies III and IV. Neurology. 1999;52:1652–7.
Macefield VG, Norcliffe-Kaufmann L, Axelrod FB, Kaufmann H. Cardiac-locked bursts of muscle sympathetic nerve activity are absent in familial dysautonomia. J Physiol. 2013;591:689–700. https://doi.org/10.1113/jphysiol.2012.246264.
Norcliffe-Kaufmann L, Axelrod F, Kaufmann H. Afferent baroreflex failure in familial dysautonomia. Neurology. 2010;75:1904–11. https://doi.org/10.1212/WNL.0b013e3181feb283.
Norcliffe-Kaufmann L, Kaufmann H. Familial dysautonomia (Riley-Day syndrome): when baroreceptor feedback fails. Auton Neurosci. 2012;172:26–30. https://doi.org/10.1016/j.autneu.2012.10.012.
Norcliffe-Kaufmann L, Martinez J, Axelrod F, Kaufmann H. Hyperdopaminergic crises in familial dysautonomia: a randomized trial of carbidopa. Neurology. 2013;80:1611–7. https://doi.org/10.1212/WNL.0b013e31828f18f0.
Axelrod FB, Zupanc M, Hilz MJ, Kramer EL. Ictal SPECT during autonomic crisis in familial dysautonomia. Neurology. 2000;55:122–5.
Clayson D, Welton W, Axelrod FB. Personality development and familial dysautonomia. Pediatrics. 1980;65(2):269–74.
Indo Y, Tsuruta M, Hayashida Y, Karim MA, Ohta K, Kawano T, et al. Mutations in the TRKA/NGF receptor gene in patients with congenital insensitivity to pain with anhidrosis. Nat Genet. 1996;13:485–8. https://doi.org/10.1038/ng0896-485.
Rekhtman Y, Bomback AS, Nash MA, Cohen SD, Matalon A, Jan DM, et al. Renal transplantation in familial dysautonomia: report of two cases and review of the literature. Clin J Am Soc Nephrol. 2010;5:1676–80. https://doi.org/10.2215/CJN.01750210.
Low PA, Burke WJ, McLeod JG. Congenital sensory neuropathy with selective loss of small myelinated fibers. Ann Neurol. 1978;3:179–82. https://doi.org/10.1002/ana.410030215.
Einarsdottir E, Carlsson A, Minde J, Toolanen G, Svensson O, Solders G, et al. A mutation in the nerve growth factor beta gene (NGFβ) causes loss of pain perception. Hum Mol Genet. 2004;13:799–805. https://doi.org/10.1093/hmg/ddh096.
Minde J, Toolanen G, Andersson T, Nennesmo I, Remahl IN, Svensson O, et al. Familial insensitivity to pain (HSAN V) and a mutation in the NGFβ gene. A neurophysiological and pathological study. Muscle Nerve. 2004;30:752–60. https://doi.org/10.1002/mus.20172.
Carvalho OP, Thornton GK, Hertecant J, Houlden H, Nicholas AK, Cox JJ, et al. A novel NGF mutation clarifies the molecular mechanism and extends the phenotypic spectrum of the HSAN5 neuropathy. J Med Genet. 2011;48:131–5. https://doi.org/10.1136/jmg.2010.081455.
Minde J, Svensson O, Holmberg M, Solders G, Toolanen G. Orthopedic aspects of familial insensitivity to pain due to a novel nerve growth factor beta mutation. Acta Orthop. 2006;77:198–202. https://doi.org/10.1080/17453670610045911.
Edvardson S, Cinnamon Y, Jalas C, Shaag A, Maayan C, Axelrod FB, et al. Hereditary sensory autonomic neuropathy caused by a mutation in dystonin. Ann Neurol. 2012;71:569–72. https://doi.org/10.1002/ana.23524.
• Manganelli F, Parisi S, Nolano M, Tao F, Paladino S, Pisciotta C, et al. Novel mutations in dystonin provide clues to the pathomechanisms of HSAN-VI. Neurology. 2017;88:2132–40. https://doi.org/10.1212/WNL.0000000000003992 The authors described another HSAN-VI family harboring two novel heterozygous mutations of DST expanding the phenotype to include a nonlethal and non-syndromic form due to a different involved isoform of dystonin other than the one Evardson et al. described in 2012.
Ichikawa H, Terayama R, Yamaai T, De Repentigny Y, Kothary R, Sugimoto T. Dystonin deficiency reduces taste buds and fungiform papillae in the anterior part of the tongue. Brain Res. 2007;1129:142–6. https://doi.org/10.1016/j.brainres.2006.04.044.
Leipold E, Liebmann L, Korenke GC, Heinrich T, Giesselmann S, Baets J, et al. A de novo gain-of-function mutation in SCN11A causes loss of pain perception. Nat Genet. 2013;45:1399–404. https://doi.org/10.1038/ng.2767.
Cummins TR, Dib-Hajj SD, Black JA, Akopian AN, Wood JN, Waxman SG. A novel persistent tetrodotoxin-resistant sodium current in SNS-null and wild-type small primary sensory neurons. J Neurosci. 1999;19:RC43.
Woods CG, Babiker MO, Horrocks I, Tolmie J, Kurth I. The phenotype of congenital insensitivity to pain due to the NaV1.9 variant p.L811P. Eur J Hum Genet. 2015;23:1434. https://doi.org/10.1038/ejhg.2015.163.
•• Salvatierra J, Diaz-Bustamante M, Meixiong J, Tierney E, Dong X, Bosmans F. A disease mutation reveals a role for NaV1.9 in acute itch. J Clin Invest. 2018;128:5434–47. https://doi.org/10.1172/JCI122481 The authors studied the role of Na V 1.9 in itching by using a Na V 1.9 −/− and Na V 1.9 L799P/WT mouse models. In the latter, pruritogens altered action potential parameters. Na V 1.9 −/− mice exhibited reduction in scratching behavior in response to pruritogens, whereas Na V 1.9 L799P/WT mice had increased spontaneous scratching.
Chen YC, Auer-Grumbach M, Matsukawa S, Zitzelsberger M, Themistocleous AC, Strom TM, et al. Transcriptional regulator PRDM12 is essential for human pain perception. Nat Genet. 2015;47:803–8. https://doi.org/10.1038/ng.3308.
• Zhang S, Malik Sharif S, Chen YC, Valente EM, Ahmed M, Sheridan E, et al. Clinical features for diagnosis and management of patients with PRDM12 congenital insensitivity to pain. J Med Genet. 2016;53:533–5. https://doi.org/10.1136/jmedgenet-2015-103646 The authors provide a thorough description of the phenotype and natural history of HSAN-VIII in five cases of PRDM12 mutations following the initial description in 2015 by Chen et al.
Auer-Grumbach M, De Jonghe P, Wagner K, Verhoeven K, Hartung HP, Timmerman V. Phenotype–genotype correlations in a CMT2B family with refined 3q13–q22 locus. Neurology. 2000;55:1552–7.
Schuster R, Stewart D, Schuster L, Greaney G, Waxman K. Preoperative oral rofecoxib and postoperative pain in patients after laparoscopic cholecystectomy: a prospective, randomized, double-blinded, placebo-controlled trial. Am Surg. 2005;71:827–9.
Auer-Grumbach M, De Jonghe P, Verhoeven K, Timmerman V, Wagner K, Hartung HP, et al. Autosomal dominant inherited neuropathies with prominent sensory loss and mutilations: a review. Arch Neurol. 2003;60:329–34.
Mauermann MLaK, C. J. Hereditary sensory and autonomic neuropathies and miscellaneous inherited neuropathies with autonomic involvement. In: Low PA and Benarroch EE, editors. Clinical autonomic disorders. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2008: 468–481.
Axelrod FB KH. Hereditary Sensory and Autonomic Neuropathies. In: Basil Darras H. Royden Jones JMRDDV, editor. Neuromuscular disorders of infancy, childhood, and adolescence. 2nd ed.: Elsevier; 2015.:340–353.
Nolano M, Crisci C, Santoro L, Barbieri F, Casale R, Kennedy WR, et al. Absent innervation of skin and sweat glands in congenital insensitivity to pain with anhidrosis. Clin Neurophysiol. 2000;111:1596–601.
Dyck PJ. Histologic measurements and fine structure of biopsied sural nerve: normal, and in peroneal muscular atrophy, hypertrophic neuropathy, and congenital sensory neuropathy. Mayo Clin Proc. 1966;41:742–74.
Minde J, Andersson T, Fulford M, Aguirre M, Nennesmo I, Remahl IN, et al. A novel NGFβ point mutation: a phenotype study of heterozygous patients. J Neurol Neurosurg Psychiatry. 2009;80:188–95. https://doi.org/10.1136/jnnp.2007.136051.
Norcliffe-Kaufmann L, Axelrod FB, Kaufmann H. Developmental abnormalities, blood pressure variability and renal disease in Riley Day syndrome. J Hum Hypertens. 2013;27:51–5. https://doi.org/10.1038/jhh.2011.107.
Axelrod FB, Liebes L, Gold-Von Simson G, Mendoza S, Mull J, Leyne M, et al. Kinetin improves IKBKAP mRNA splicing in patients with familial dysautonomia. Pediatr Res. 2011;70:480–3. https://doi.org/10.1203/PDR.0b013e31822e1825.
Slaugenhaupt SA, Mull J, Leyne M, Cuajungco MP, Gill SP, Hims MM, et al. Rescue of a human mRNA splicing defect by the plant cytokinin kinetin. Hum Mol Genet. 2004;13:429–36. https://doi.org/10.1093/hmg/ddh046.
Axelrod FB, Berlin D. Pregabalin: a new approach to treatment of the dysautonomic crisis. Pediatrics. 2009;124:743–6. https://doi.org/10.1542/peds.2008-3318.
Axelrod FB. Familial dysautonomia: a review of the current pharmacological treatments. Expert Opin Pharmacother. 2005;6:561–7. https://doi.org/10.1517/14656566.6.4.561.
Axelrod FB M. Familial dysautonomia. 17th ed. Gellis and Kagen’s current pediatric therapy. 2002.
• Spalink CL, Barnes E, Palma JA, Norcliffe-Kaufmann L, Kaufmann H. Intranasal dexmedetomidine for adrenergic crisis in familial dysautonomia. Clin Auton Res. 2017;27:279–82. https://doi.org/10.1007/s10286-017-0442-6 The authors reported in this pilot study that Intranasal dexmedetomidine is safe and feasible in acute treatment of adrenergic crisis in patients with HSAN-III.
Axelrod FB, Goldberg JD, Rolnitzky L, Mull J, Mann SP, Gold von Simson G, et al. Fludrocortisone in patients with familial dysautonomia—assessing effect on clinical parameters and gene expression. Clin Auton Res. 2005;15:284–91. https://doi.org/10.1007/s10286-005-0288-1.
Auer-Grumbach M. Hereditary sensory neuropathy type I. Orphanet J Rare Dis. 2008;3:7. https://doi.org/10.1186/1750-1172-3-7.
Kazachkov M, Palma JA, Norcliffe-Kaufmann L, Bar-Aluma BE, Spalink CL, Barnes EP, et al. Respiratory care in familial dysautonomia: systematic review and expert consensus recommendations. Respir Med. 2018;141:37–46. https://doi.org/10.1016/j.rmed.2018.06.017.
Mass E. A review of the oro-dento-facial characteristics of hereditary sensory and autonomic neuropathy type III (familial dysautonomia). Spec Care Dentist. 2012;32:15–20. https://doi.org/10.1111/j.1754-4505.2011.00225.x.
Sands SA, Giarraffa P, Jacobson CM, Axelrod FB. Familial dysautonomia’s impact on quality of life in childhood, adolescence, and adulthood. Acta Paediatr. 2006;95:457–62. https://doi.org/10.1080/08035250500440386.
Anderson SL, Qiu J, Rubin BY. Tocotrienols induce IKBKAP expression: a possible therapy for familial dysautonomia. Biochem Biophys Res Commun. 2003;306:303–9.
Lee G, Papapetrou EP, Kim H, Chambers SM, Tomishima MJ, Fasano CA, et al. Modelling pathogenesis and treatment of familial dysautonomia using patient-specific iPSCs. Nature. 2009;461:402–6. https://doi.org/10.1038/nature08320.
Hims MM, Ibrahim EC, Leyne M, Mull J, Liu L, Lazaro C, et al. Therapeutic potential and mechanism of kinetin as a treatment for the human splicing disease familial dysautonomia. J Mol Med (Berlin). 2007;85:149–61. https://doi.org/10.1007/s00109-006-0137-2.
Keren H, Donyo M, Zeevi D, Maayan C, Pupko T, Ast G. Phosphatidylserine increases IKBKAP levels in familial dysautonomia cells. PLoS One. 2010;5:e15884. https://doi.org/10.1371/journal.pone.0015884.
Cheishvili D, Maayan C, Holzer N, Tsenter J, Lax E, Petropoulos S, et al. Tocotrienol treatment in familial dysautonomia: open-label pilot study. J Mol Neurosci. 2016;59:382–91. https://doi.org/10.1007/s12031-016-0760-5.
Boone N, Loriod B, Bergon A, Sbai O, Formisano-Treziny C, Gabert J, et al. Olfactory stem cells, a new cellular model for studying molecular mechanisms underlying familial dysautonomia. PLoS One. 2010;5:e15590. https://doi.org/10.1371/journal.pone.0015590.
Gold-von Simson G, Goldberg JD, Rolnitzky LM, Mull J, Leyne M, Voustianiouk A, et al. Kinetin in familial dysautonomia carriers: implications for a new therapeutic strategy targeting mRNA splicing. Pediatr Res. 2009;65:341–6. https://doi.org/10.1203/PDR.0b013e318194fd52.
Gold-von Simson G, Leyne M, Mull J, Rolnitzky LM, Goldberg JD, Berlin D, et al. IKBKAP mRNA in peripheral blood leukocytes: a molecular marker of gene expression and splicing in familial dysautonomia. Pediatr Res. 2008;63:186–90. https://doi.org/10.1203/PDR.0b013e31815ef74b.
Jun BK, Chandra A, Kuljis D, Schmidt BP, Eichler FS. Substrate availability of mutant SPT alters neuronal branching and growth cone dynamics in dorsal root ganglia. J Neurosci. 2015;35:13713–9. https://doi.org/10.1523/JNEUROSCI.1403-15.2015.
Garofalo K, Penno A, Schmidt BP, Lee HJ, Frosch MP, von Eckardstein A, et al. Oral L-serine supplementation reduces production of neurotoxic deoxysphingolipids in mice and humans with hereditary sensory autonomic neuropathy type 1. J Clin Invest. 2011;121:4735–45. https://doi.org/10.1172/JCI57549.
•• Fridman V, Suriyanarayanan S, Novak P, David W, Macklin EA, McKenna-Yasek D, et al. Randomized trial of l-serine in patients with hereditary sensory and autonomic neuropathy type 1. Neurology. 2019;92:e359–e70. https://doi.org/10.1212/WNL.0000000000006811 This randomized, placebo-controlled trial proved that high-dose oral l -serine is safe and potentially effective at slowing disease progression in patients with HSAN1 (Class I evidence).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
M.K. reports personal fees from Akcea Therapeutics, outside the submitted work. C.S. declares no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Autonomic Dysfunction
Rights and permissions
About this article
Cite this article
Schwartzlow, C., Kazamel, M. Hereditary Sensory and Autonomic Neuropathies: Adding More to the Classification. Curr Neurol Neurosci Rep 19, 52 (2019). https://doi.org/10.1007/s11910-019-0974-3
Published:
DOI: https://doi.org/10.1007/s11910-019-0974-3