Abstract
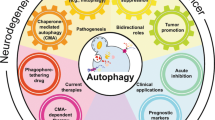
Autophagy is a major intracellular degradative process that delivers cytoplasmic materials to the lysosome for degradation. Since the discovery of autophagy-related (Atg) genes in the 1990s, there has been a proliferation of studies on the physiological and pathological roles of autophagy in a variety of autophagy knockout models. However, direct evidence of the connections between ATG gene dysfunction and human diseases has emerged only recently. There are an increasing number of reports showing that mutations in the ATG genes were identified in various human diseases such as neurodegenerative diseases, infectious diseases, and cancers. Here, we review the major advances in identification of mutations or polymorphisms of the ATG genes in human diseases. Current autophagy-modulating compounds in clinical trials are also summarized.
Similar content being viewed by others
Introduction
Half a century ago, Christian de Duve coined the term “autophagy” (literally, “self-eating” in Greek) to describe a process where the cell digests its cytoplasmic materials within lysosomes1. At least three major types of autophagy have been identified: macroautophagy, characterized by the formation of a unique double-membrane organelle called the autophagosome; microautophagy, where lysosomes engulf cytoplasmic materials by inward invagination of the lysosomal membrane; and chaperone-mediated autophagy, mediated by the chaperone hsc70, co-chaperones, and the lysosomal-associated membrane protein type 2A2,3. This review focuses on the role of macroautophagy (hereafter referred to as autophagy) in human diseases.
In recent years, genetic deletion of the autophagy-related (Atg) genes in various model organisms, including mammals, has revealed that autophagy plays critical roles in adaptive responses to starvation and other forms of stress, homeostasis, and cellular differentiation and development2,4,5,6,7. In addition, analysis of mice with systemic or tissue-specific deletion of Atg genes has revealed the connection between dysregulated autophagy and various kinds of disease-like phenotypes including cancer, neurodegenerative diseases, infectious diseases, and metabolic diseases2,6,7,8,9,10,11. However, these experimental results do not directly demonstrate that defects in autophagy contribute to pathogenesis of human diseases. Thus, it has become particularly important to understand the genetic basis of putative human autophagy-related diseases.
With the completion of the Human Genome Project in 2003 and the International HapMap Project in 2005, researchers now have a powerful set of research tools, including the high-speed DNA sequencing technology that make it possible to identify the genetic contributions to specific diseases, even if they are rare. Indeed, genome-wide studies have identified disease-associated loci and genes in many human diseases. Table 1 summarizes the association between genetic variants of autophagy-related genes and selected human diseases.
Static encephalopathy of childhood with neurode-generation in adulthood (SENDA)
Recently, two groups identified de novo mutations in WDR45, an autophagy-related gene located at Xp11.23, in individuals with SENDA by whole-exome sequencing using next-generation sequencing technologies12,13. SENDA is a recently established subtype of neurode-generation with brain iron accumulation14 that begins with early-onset spastic paraplegia and mental retardation, which remain static until adulthood. Patients subsequently develop sudden-onset parkinsonism and dystonia during their late 20s to early 30s. Additional features include eye movement abnormalities, frontal release signs, sleep disorders, and dysautonomia. Brain magnetic resonance imaging has revealed iron accumulation in the globus pallidus and hypointensity in the substantia nigra, as well as white matter changes14,15.
The hit gene WDR45 (also known as WIPI4) is one of the four mammalian homologues of yeast Atg18, which plays an important role in autophagosome formation16,17,18,19. Atg18/WIPIs belong to the PROPPIN family of proteins. They contain seven-bladed β-propellers formed by seven WD40 repeats and bind to phosphatidylinositol 3-phosphate and the lysosomal/vacuolar lipid phosphatidylinositol 3,5-bisphosphate (PtdIns(3,5)P2)17,20. Atg18/WIPIs also interact with Atg220,21,22. The crystal structure of Hsv2, a yeast Atg18 paralogue, shows two phosphoinositide-binding sites at blades five and six, and an Atg2-binding region at blade 223,24,25. Atg18/WIPIs are recruited to the autophagosome formation site through binding to phosphatidylinositol 3-phosphate, which is synthesized by the class III PtdIns 3-kinase complex18,21. Caenorhabditis elegans has two Atg18 homologues, ATG-18 and EPG-619. Interestingly, C. elegans requires both ATG-18 and EPG-6 for autophagy because the two molecules function sequentially, not redundantly. Human WDR45/WIPI4 shows a higher similarity to EPG-6 than to ATG-18, and loss of epg-6/WIPI4 causes the accumulation of premature autophagic structures in both C. elegans and mammalian cells19. In fact, by using lymphoblastoid cell lines derived from SENDA patients, Saitsu et al. confirmed that the protein expression of WIPI4 was severely reduced in affected individuals. Specifically, blocked autophagic flux and accumulation of abnormal ATG9A- and LC3-double-positive structures, which may represent aberrant early autophagic structures, were observed in the lymphoblastoid cell lines of affected individuals13. Since WDR45/WIPI4 is encoded by the X chromosome and one of the X chromosomes is subjected to X inactivation, female patients should possess mosaic loss of function of WDR45/WIPI4. It is unclear, however, whether hemizygous mutations in male patients are lethal. Hayflick's group reported three male SENDA patients with similar phenotypes12,26; all three may have had somatic mosaicism.
These studies provided the first direct evidence that the deficiency of a core autophagy factor is indeed a contributing factor to human neurodegenerative diseases. However, the exact mechanism of brain iron accumulation due to an autophagy defect and why only the brain is affected remain to be clarified. Further investigation of these aspects is needed.
Vici syndrome
A recent study by Cullup et al. showed that recessive mutations in EPG5, a key factor implicated in the maturation of autolysosomes, play a causative role in Vici syndrome27. Vici syndrome is a recessively inherited multisystem disorder characterized by callosal agenesis, cataracts, hypopigmentation, cardiomyopathy, psychomotor retardation, and immunodeficiency with cleft lip and palate28,29,30,31.
EPG5 is a metazoan-specific autophagy gene first identified by genetically screening C. elegans for mutants with defective degradation of autophagy substrates. C. elegans epg-5 mutant and knockdown of mEPG5 in mammalian cells show accumulation of non-degradative autolysosomes, indicating the role of EPG-5/mEPG5 in autolysosome maturation32. It was later shown that knockdown of EPG5 in HeLa cells results in another defect in the endocytic pathway33. By using fibroblasts derived from patients with Vici syndrome, Cullup et al. showed that autophagic flux is blocked and the autophagy adapters NBR1 and SQSTM1/p62 accumulate, confirming the decreased autophagic activity in Vici syndrome27. However, as EPG5 is also involved in the endocytic pathway, it is important to examine whether dysregulated endocytic trafficking also contributes to the pathogenesis of Vici syndrome. Furthermore, the Epg5-deficient mice display only some features of Vici syndrome33,34. For example, although patients with Vici syndrome demonstrate facial dysmorphism and cataracts, these features are not marked in the Epg5-deficient mice. In addition, psychomotor abnormalities appear to be milder in mice than in humans. Further studies are needed to elucidate the reason for phenotypic differences between mice and humans as well as the exact molecular role of EPG5 in the autophagy and endocytic pathways.
Hereditary spastic paraparesis
Oz-Levi et al. reported a recessive mutation in TECPR2, an autophagy-related WD repeat-containing protein, in five individuals with SPG49, a novel form of recessive hereditary spastic paraparesis (HSP)35. HSP is a diverse group of neurodegenerative disorders characterized by axonal degeneration of the corticospinal or pyramidal motor and sensory tracts that control the lower extremities. It leads to progressive spasticity and hyperreflexia of the lower limbs36,37,38. The newly characterized HSP subtype, accompanied by lower-limb spasticity and other neurological symptoms, appears to be an autosomal-recessive form of complicated HSP that is caused by a single base deletion in the TECPR2 gene, resulting in a premature stop codon accompanied by full degradation of its protein product35.
TECPR2, an uncharacterized protein belonging to the tectonin β-propeller repeat-containing protein family, was previously found to interact with ATG8 orthologues, suggesting a possible role in the autophagy pathway39. Skin fibroblasts from an HSP patient showed decreased autophagic flux, but no accumulation of the autophagic substrate SQSTM1/p62, implying that some autophagic activity could be maintained in affected individuals. Knockdown of TECPR2 in HeLa cells also reduced autophagic activity, suggesting that TECPR2 is a bona fide autophagy factor35. However, the exact role of TECPR2 in the autophagy pathway warrants further examination. The fact that TECPR2 shows some similarity to two autophagy-involved proteins — TECPR1 and HPS535,40,41,42,43 — is expected to shed new light on this issue.
Recently, Vantaggiato et al. reported that ZFYVE26/SPG15, the causative gene of another recessive complicated form of HSP (HSP type 15), is also involved in the autophagy process44. ZFYVE26/SPG15 encodes a zinc-finger protein with a FYVE domain and a leucine zipper, termed spastizin45. Spastizin interacts with the Beclin 1-UVRAG-Rubicon complex and mediates autophagosome maturation. Both spastizin-mutated fibroblast cells derived from HSP patients and spastizin knockdown cells showed impaired autophagic flux and accumulation of autophagosomes due to reduced autophagosome–lysosome fusion44. However, as this complex also plays an important role in the endocytic pathway46,47,48,49, and as spastizin is not present on the autophagic membranes44, whether spastizin specifically regulates autophagosome-lysosome fusion needs to be clarified.
Parkinson's disease
Parkinson's disease is the most common form of a group of progressive neurodegenerative disorders characterized clinically by bradykinesia (paucity and slowness of movement), rest tremor, muscular rigidity, shuffling gait, and flexed posture. It can also be accompanied by various non-motor symptoms, including sleep, autonomic, sensory, cognitive, and psychiatric disturbances. Nearly all forms of Parkinson's disease result from reduced dopaminergic transmission in the basal ganglia50,51. Many genes, mutations, and polymorphisms have been implicated in the pathogenesis of the disease. Among them, mutations in the PARK2/Parkin and PARK6/PINK1 have been shown to lead to autosomal recessive or sporadic juvenile-onset Parkinson's disease52,53,54.
PTEN-induced putative kinase protein 1 (PINK1, encoded by PARK6/PINK1) is a mitochondria-associated protein kinase that acts upstream of Parkin (encoded by PARK2/Parkin), an E3 ubiquitin ligase implicated in the selective degradation of damaged mitochondria by autophagy, a process termed “mitophagy”55,56,57. When mitochondria are damaged and lose their membrane potential, mitochondrial PINK1 is stabilized and recruits Parkin, which ubiquitinates a number of mitochondrial membrane proteins, resulting in selective mitophagy. Consistent with this finding, excessive mitochondrial damage has been linked to Parkinson's disease58. Thus, this type of Parkinson's disease can be caused by the accumulation of mitochondrial damage. However, Parkin is also reported to mediate other biological processes, including translocation of some mitochondrial outer membrane proteins to the endoplasmic reticulum to escape autophagic degradation59. Furthermore, other studies have shown that Parkin also mediates proteasome-dependent degradation of outer membrane proteins of depolarized mitochondria, although it is controversial whether this process is required for mitophagy60,61,62, these findings suggest that an autophagic defect may not be the only factor contributing to the pathogenesis of PINK1/Parkin-related Parkinson's disease. It would also be important to know whether PINK1/Parkin-mediated mitophagy occurs under physiological conditions, because most previous studies were performed in cells overexpressing Parkin, and PINK1/Parkin knockout mice failed to faithfully recapitulate Parkinson's disease in humans63,64,65.
Lysosomal storage disorders
Lysosomal storage disorders (LSDs), characterized by progressive accumulation of undigested macromolecules within the cell, are a family of disorders caused by inherited gene mutations that perturb lysosomal homeostasis. As lysosomes also play an important role in the autophagy pathway by fusing with autophagosomes and degrading autophagic cargo, lysosomal dysfunction in LSDs impacts the autophagy pathway. In fact, in most LSDs, the lysosomal dysfunction is accompanied by impaired autophagic flux, resulting in defective autophagosome-lysosome fusion and secondary accumulation of autophagy substrates such as SQSTM1/p62, polyubiquitinated proteins, and damaged mitochondria66. In some sense then, LSDs can be regarded as “autophagy disorders”. Some excellent reviews on the genetic basis of LSDs are available11,67,68.
Cancer
An association between autophagy and cancer has long been proposed. The role of autophagy likely differs in different stages of cancer development; initially, autophagy probably has a preventive effect against cancer, but once a tumor develops, the cancer cells could utilize autophagy for their own cytoprotection9,69.
Monoallelic deletion of BECN1 has been detected in human breast, ovarian, and prostate tumor specimens70,71,72,73. In particular, the aberrant expression of Beclin 1 (encoded by the human BECN1 gene) in many kinds of tumor tissues correlates with poor prognosis74,75,76,77,78. Beclin 1, the mammalian orthologue of yeast Atg6/vacuolar protein sorting (Vps)-30, plays an essential role in autophagy. It interacts with the class III PtdIns 3-kinase, Vps34 (also known as PIK3C3 in mammals), to form the Beclin 1-Atg14-Vps34-Vps15 complex, which is important for the localization of downstream autophagic proteins to the autophagosome formation site to induce autophagy73,79. Beclin 1 also has other important biological functions including roles in anti-apoptosis80,81 and endocytic trafficking47,82,83.
A recent study in C. elegans identified EI24/PIG8, whose human homolog was reported to be mutated in breast cancers84, as a critical factor of autophagic degradation32. However, it remains to be clarified whether EI24-mutated human breast cancer cells indeed show decreased autophagic activity. Furthermore, since EI24/PIG8 is also known as the proapoptotic factor84,85, this role may contribute to tumor suppression. Besides Beclin 1 and EI24, altered expression of several autophagy proteins such as ATG586,87, and UVRAG88 are reported to be associated with human cancers7,89.
Crohn's disease
Genome-wide association studies of non-synonymous SNPs have linked ATG16L1 variants with susceptibility to Crohn's disease90,91, a major type of inflammatory bowel disease that can affect any part of the digestive tract from the mouth to the anus. The disease causes a wide variety of symptoms including abdominal pain, diarrhea, vomiting, and weight loss, as well as complications outside the gastrointestinal tract such as fatigue, skin rash, inflammation of the eye, anemia, arthritis, and lack of concentration92.
Atg16L1, a core component of the autophagy machinery, forms a complex with Atg12-Atg5 to induce LC3 lipidation and is essential for autophagosome formation93,94. Recent studies have shown that the interaction between Atg16L1 and FIP200 is important for the localization of the Atg12-Atg5-Atg16L1 complex to the autophagosome formation site or isolation membrane95,96. The Atg16L1 protein possesses a C-terminal WD repeat domain, and the Crohn's disease-associated mutation (T300A, also known as Ala197Thr) is within or immediately upstream of this domain. However, it was shown that the Atg16L1 WD repeat domain is not essential for autophagic activity96,97. Thus, it is important to clarify how the ATG16L1 T300A mutation contributes to the pathogenesis of Crohn's disease in humans.
Investigations of mice carrying two distinct mutations that reduce or eliminate the expression of Atg16L1 have suggested potential links between Atg16L1 mutations and Crohn's disease. It was shown that Atg16L1-deficient macrophages produced more of the inflammatory cytokines IL-1β and IL-18 upon stimulation with lipopolysaccharides98. On the other hand, the Atg16L1 hypomorph mice exhibited aberrant granule formation in Paneth cells, which play an important role in the innate immune response of the intestine99. Recently, Marchiando et al. reported that Atg16L1 possesses an immunosuppressive role during intestinal bacterial infection100.
Apart from Atg16L1, other autophagy-related proteins such as IRGM101,102,103 and NOD2104,105,106 are reported to be associated with Crohn's disease in humans107. However, since these proteins also play roles in biological processes other than autophagy, it remains unclear whether they relate to Crohn's disease via autophagy modulation.
Conclusion and future prospects
In this article, we have summarized recent findings on the relationship between autophagy and human diseases. It is expected that new efficient technologies such as exome sequencing will help to identify more autophagy-related diseases over the next few years. Given that autophagy is associated with a plethora of human diseases, there are at least two important issues to address.
First, the development of pharmacological agents that modulate autophagy in these pathological conditions is critical; in fact, it has become a major priority in the field. Pharmacological approaches to activate or inhibit autophagy are also required because autophagy can play either a protective or destructive role in different diseases, even in different stages of the same diseases. Many drugs and compounds that modulate autophagy are currently receiving considerable attention11,89,108. These include, for example, autophagy inducers such as the mTORC1 inhibitor rapamycin109 and its analogues (e.g., CCI-779109, RAD001110,111, and AP23573112), mTOR kinase inhibitors (e.g., Torin 1113, and PP242114), trehalose115,116, carbamazepine117, and the newly identified autophagy-inducing peptide Tat–beclin 1118; autophagy inhibitors such as chloroquine119,120 and hydroxychloroquine121, Lys05122, 3-methyladenine123 and its derivatives124, PIK3C3 inhibitors125, ATG4B inhibitors126,127, and ATG7 inhibitors128,129. Autophagy-modulating drugs that are currently used in clinical trials are summarized in Table 2. An improved understanding of how autophagy defects contribute to the pathogenesis of human diseases and the development of other more specific and less toxic compounds will benefit many more patients.
Second, and perhaps a more challenging issue, is the monitoring of autophagic activity in humans, in tissue samples at the least, but preferably in blood samples. In particular, it is more important to measure autophagic flux than autophagosome number. To date, however, measurement of autophagic flux in paraffin-embedded tissue samples has been unsuccessful, and the simple detection of endogenous LC3-II, a commonly used marker for autophagosomes, has proved problematic in tissue sections. The appearance of more LC3-positive puncta (which may represent autophagosomes) does not necessarily indicate higher autophagic activity in the tissue. Autophagosomes can accumulate due to the induction of autophagy or due to blocking of a late step of the autophagy pathway, including impaired autophagosome-lysosome fusion and compromised lysosomal activity130. This is a frequent occurrence in human diseases and even during the normal aging process. It should also be remembered that LC3 can be incorporated into protein aggregates independently of autophagy131. To help overcome these problems, it may be beneficial to combine immunohistochemical assays of other autophagy-related marker proteins such as ATG5 and Beclin 1 to detect autophagy in clinical tissue samples.
References
de Duve C, Wattiaux R . Functions of lysosomes. Annu Rev Physiol 1966; 28:435–492.
Mizushima N, Komatsu M . Autophagy: renovation of cells and tissues. Cell 2011; 147:728–741.
Kaushik S, Cuervo AM . Chaperone-mediated autophagy: a unique way to enter the lysosome world. Trends Cell Biol 2012; 22:407–417.
Mizushima N, Levine B . Autophagy in mammalian development and differentiation. Nat Cell Biol 2010; 12:823–830.
Rabinowitz JD, White E . Autophagy and metabolism. Science 2010; 330:1344–1348.
Levine B, Mizushima N, Virgin HW . Autophagy in immunity and inflammation. Nature 2011; 469:323–335.
Choi AM, Ryter SW, Levine B . Autophagy in human health and disease. N Engl J Med 2013; 368:651–662.
Rubinsztein DC, Mariño G, Kroemer G . Autophagy and aging. Cell 2011; 146:682–695.
White E . Deconvoluting the context-dependent role for autophagy in cancer. Nat Rev Cancer 2012; 12:401–410.
Murrow L, Debnath J . Autophagy as a stress-response and quality-control mechanism: implications for cell injury and human disease. Annu Rev Pathol Mech Dis 2013; 8:105–137.
Nixon RA . The role of autophagy in neurodegenerative disease. Nat Med 2013; 19:983–997.
Haack TB, Hogarth P, Kruer MC, et al. Exome sequencing reveals de novo WDR45 mutations causing a phenotypically distinct, X-linked dominant form of NBIA. Am J Hum Genet 2012; 91:1144–1149.
Saitsu H, Nishimura T, Muramatsu K, et al. De novo mutations in the autophagy gene WDR45 cause static encephalopathy of childhood with neurodegeneration in adulthood. Nat Genet 2013; 45:445–449.
Schneider SA, Bhatia KP . Syndromes of neurodegeneration with brain iron accumulation. Semin Pediatr Neurol 2012; 19:57–66.
Schneider S, Zorzi G, Nardocci N . Pathophysiology and treatment of neurodegeneration with brain iron accumulation in the pediatric population. Curr Treat Options Neurol 2013; 15:652–667.
Guan J, Stromhaug PE, George MD, et al. Cvt18/Gsa12 is required for cytoplasm-to-vacuole transport, pexophagy, and autophagy in Saccharomyces cerevisiae and Pichia pastoris. Mol Biol Cell 2001; 12:3821–3838.
Proikas-Cezanne T, Waddell S, Gaugel A, et al. WIPI-1α (WIPI49), a member of the novel 7-bladed WIPI protein family, is aberrantly expressed in human cancer and is linked to starvation-induced autophagy. Oncogene 2004; 23:9314–9325.
Polson HE, de Lartigue J, Rigden DJ, et al. Mammalian Atg18 (WIPI2) localizes to omegasome-anchored phagophores and positively regulates LC3 lipidation. Autophagy 2010; 6:506–522.
Lu Q, Yang P, Huang X, et al. The WD40 repeat PtdIns(3)P-binding protein EPG-6 regulates progression of omegasomes to autophagosomes. Dev Cell 2011; 21:343–357.
Dove SK, Piper RC, McEwen RK, et al. Svp1p defines a family of phosphatidylinositol 3,5-bisphosphate effectors. EMBO J 2004; 23:1922–1933.
Obara K, Sekito T, Niimi K, Ohsumi Y . The Atg18-Atg2 complex is recruited to autophagic membranes via phosphatidylinositol 3-phosphate and exerts an essential function. J Biol Chem 2008; 283:23972–23980.
Velikkakath AK, Nishimura T, Oita E, Ishihara N, Mizushima N . Mammalian Atg2 proteins are essential for autophagosome formation and important for regulation of size and distribution of lipid droplets. Mol Biol Cell 2012; 23:896–909.
Baskaran S, Ragusa MJ, Boura E, Hurley JH . Two-site recognition of phosphatidylinositol 3-phosphate by PROPPINs in autophagy. Mol Cell 2012; 47:339–348.
Krick R, Busse RA, Scacioc A, et al. Structural and functional characterization of the two phosphoinositide binding sites of PROPPINs, a β-propeller protein family. Proc Natl Acad Sci USA 2012; 109:E2042–2049.
Watanabe Y, Kobayashi T, Yamamoto H, et al. Structure-based analyses reveal distinct binding sites for Atg2 and phosphoinositides in Atg18. J Biol Chem 2012; 287:31681–31690.
Hayflick SJ, Kruer MC, Gregory A, et al. Beta-propeller protein-associated neurodegeneration: a new X-linked dominant disorder with brain iron accumulation. Brain 2013; 136:1708–1717.
Cullup T, Kho AL, Dionisi-Vici C, et al. Recessive mutations in EPG5 cause Vici syndrome, a multisystem disorder with defective autophagy. Nat Genet 2013; 45:83–87.
del Campo M, Hall BD, Aeby A, et al. Albinism and agenesis of the corpus callosum with profound developmental delay: Vici syndrome, evidence for autosomal recessive inheritance. Am J Med Genet 1999; 85:479–485.
Chiyonobu T, Yoshihara T, Fukushima Y, et al. Sister and brother with Vici syndrome: agenesis of the corpus callosum, albinism, and recurrent infections. Am J Med Genet 2002; 109:61–66.
Özkale M, Erol I, Gümüş A, Özkale Y, Alehan F . Vici syndrome associated with sensorineural hearing loss and laryngomalacia. Pediatr Neurol 2012; 47:375–378.
Said E, Soler D, Sewry C . Vici syndrome—A rapidly progressive neurodegenerative disorder with hypopigmentation, immunodeficiency and myopathic changes on muscle biopsy. Am J Med Genet A 2012; 158A:440–444.
Tian Y, Li Z, Hu W, et al. C. elegans screen identifies autophagy genes specific to multicellular organisms. Cell 2010; 141:1042–1055.
Zhao H, Zhao YG, Wang X, et al. Mice deficient in Epg5 exhibit selective neuronal vulnerability to degeneration. J Cell Biol 2013; 200:731–741.
Zhao YG, Zhao H, Sun H, Zhang H . Role of Epg5 in selective neurodegeneration and Vici syndrome. Autophagy 2013; 9:1258–1262.
Oz-Levi D, Ben-Zeev B, Ruzzo EK, et al. Mutation in TECPR2 reveals a role for autophagy in hereditary spastic paraparesis. Am J Hum Genet 2012; 91:1065–1072.
Depienne C, Stevanin G, Brice A, Durr A . Hereditary spastic paraplegias: an update. Curr Opin Neurol 2007; 20:674–680.
Schüle R, Schöls L . Genetics of hereditary spastic paraplegias. Semin Neurol 2011; 31:484–493.
Blackstone C . Cellular pathways of hereditary spastic paraplegia. Annu Rev Neurosci 2012; 35:25–47.
Behrends C, Sowa ME, Gygi SP, Harper JW . Network organization of the human autophagy system. Nature 2010; 466:68–76.
Ogawa M, Yoshikawa Y, Kobayashi T, et al. A Tecpr1-dependent selective autophagy pathway targets bacterial pathogens. Cell Host Microbe 2011; 9:376–389.
Chen D, Fan W, Lu Y, et al. A mammalian autophagosome maturation mechanism mediated by TECPR1 and the Atg12-Atg5 conjugate. Mol Cell 2012; 45:629–641.
Huizing M, Hess R, Dorward H, et al. Cellular, molecular and clinical characterization of patients with Hermansky-Pudlak syndrome type 5. Traffic 2004; 5:711–722.
Helip-Wooley A, Westbroek W, Dorward HM, et al. Improper trafficking of melanocyte-specific proteins in Hermansky-Pudlak syndrome type-5. J Invest Dermatol 2007; 127:1471–1478.
Vantaggiato C, Crimella C, Airoldi G, et al. Defective autophagy in spastizin mutated patients with hereditary spastic paraparesis type 15. Brain 2013; 136:3119–3139.
Hanein S, Martin E, Boukhris A, et al. Identification of the SPG15 gene, encoding spastizin, as a frequent cause of complicated autosomal-recessive spastic paraplegia, including Kjellin syndrome. Am J Hum Genet 2008; 82:992–1002.
Itakura E, Kishi C, Inoue K, Mizushima N . Beclin 1 forms two distinct phosphatidylinositol 3-kinase complexes with mammalian Atg14 and UVRAG. Mol Biol Cell 2008; 19:5360–5372.
Matsunaga K, Saitoh T, Tabata K, et al. Two Beclin 1-binding proteins, Atg14L and Rubicon, reciprocally regulate autophagy at different stages. Nat Cell Biol 2009; 11:385–396.
Sun Q, Westphal W, Wong KN, Tan I, Zhong Q . Rubicon controls endosome maturation as a Rab7 effector. Proc Natl Acad Sci USA 2010; 107:19338–19343.
Lee G, Liang C, Park G, et al. UVRAG is required for organ rotation by regulating Notch endocytosis in Drosophila. Dev Biol 2011; 356:588–597.
Fahn S . Description of Parkinson's disease as a clinical syndrome. Ann N Y Acad Sci 2003; 991:1–14.
Trinh J, Farrer M . Advances in the genetics of Parkinson disease. Nat Rev Neurol 2013; 9:445–454.
Kitada T, Asakawa S, Hattori N, et al. Mutations in the parkin gene cause autosomal recessive juvenile parkinsonism. Nature 1998; 392:605–608.
Valente EM, Bentivoglio AR, Dixon PH, et al. Localization of a novel locus for autosomal recessive early-onset parkinsonism, PARK6, on human chromosome 1p35-p36. Am J Hum Genet 2001; 68:895–900.
Valente EM, Abou-Sleiman PM, Caputo V, et al. Hereditary early-onset Parkinson's disease caused by mutations in PINK1. Science 2004; 304:1158–1160.
Narendra D, Tanaka A, Suen DF, Youle RJ . Parkin is recruited selectively to impaired mitochondria and promotes their autophagy. J Cell Biol 2008; 183:795–803.
Matsuda N, Sato S, Shiba K, et al. PINK1 stabilized by mitochondrial depolarization recruits Parkin to damaged mitochondria and activates latent Parkin for mitophagy. J Cell Biol 2010; 189:211–221.
Youle RJ, Narendra DP . Mechanisms of mitophagy. Nat Rev Mol Cell Biol 2011; 12:9–14.
Schapira AH . Mitochondria in the aetiology and pathogenesis of Parkinson's disease. Lancet Neurol 2008; 7:97–109.
Saita S, Shirane M, Nakayama KI . Selective escape of proteins from the mitochondria during mitophagy. Nat Commun 2013; 4:1410.
Tanaka A, Cleland MM, Xu S, et al. Proteasome and p97 mediate mitophagy and degradation of mitofusins induced by Parkin. J Cell Biol 2010; 191:1367–1380.
Chan NC, Salazar AM, Pham AH, et al. Broad activation of the ubiquitin-proteasome system by Parkin is critical for mitophagy. Hum Mol Genet 2011; 20:1726–1737.
Yoshii SR, Kishi C, Ishihara N, Mizushima N . Parkin mediates proteasome-dependent protein degradation and rupture of the outer mitochondrial membrane. J Biol Chem 2011; 286:19630–19640.
Goldberg MS, Fleming SM, Palacino JJ, et al. Parkin-deficient mice exhibit nigrostriatal deficits but not loss of dopaminergic neurons. J Biol Chem 2003; 278:43628–43635.
Perez FA, Palmiter RD . Parkin-deficient mice are not a robust model of parkinsonism. Proc Natl Acad Sci USA 2005; 102:2174–2179.
Kitada T, Tong Y, Gautier CA, Shen J . Absence of nigral degeneration in aged parkin/DJ-1/PINK1 triple knockout mice. J Neurochem 2009; 111:696–702.
Lieberman AP, Puertollano R, Raben N, et al. Autophagy in lysosomal storage disorders. Autophagy 2012; 8:719–730.
Platt FM, Boland B, van der Spoel AC . Lysosomal storage disorders: the cellular impact of lysosomal dysfunction. J Cell Biol 2012; 199:723–734.
Boustany RM . Lysosomal storage diseases—the horizon expands. Nat Rev Neurol 2013; 9:583–598.
Janku F, McConkey DJ, Hong DS, Kurzrock R . Autophagy as a target for anticancer therapy. Nat Rev Clin Oncol 2011; 8:528–539.
Saito H, Inazawa J, Saito S, et al. Detailed deletion mapping of chromosome 17q in ovarian and breast cancers: 2-cM region on 17q21.3 often and commonly deleted in tumors. Cancer Res 1993; 53:3382–3385.
Gao X, Zacharek A, Salkowski A, et al. Loss of heterozygosity of the BRCA1 and other loci on chromosome 17q in human prostate cancer. Cancer Res 1995; 55:1002–1005.
Aita VM, Liang XH, Murty VV, et al. Cloning and genomic organization of beclin 1, a candidate tumor suppressor gene on chromosome 17q21. Genomics 1999; 59:59–65.
Liang XH, Jackson S, Seaman M, et al. Induction of autophagy and inhibition of tumorigenesis by beclin 1. Nature 1999; 402:672–676.
Shi YH, Ding ZB, Zhou J, Qiu SJ, Fan J . Prognostic significance of Beclin 1-dependent apoptotic activity in hepatocellular carcinoma. Autophagy 2009; 5:380–382.
Koukourakis MI, Giatromanolaki A, Sivridis E, et al. Beclin 1 over- and underexpression in colorectal cancer: distinct patterns relate to prognosis and tumour hypoxia. Br J Cancer 2010; 103:1209–1214.
Wan XB, Fan XJ, Chen MY, et al. Elevated Beclin 1 expression is correlated with HIF-1α in predicting poor prognosis of nasopharyngeal carcinoma. Autophagy 2010; 6:395–404.
Giatromanolaki A, Koukourakis MI, Koutsopoulos A, et al. High Beclin 1 expression defines a poor prognosis in endometrial adenocarcinomas. Gynecol Oncol 2011; 123:147–151.
Xia P, Wang JJ, Zhao BB, Song CL . The role of beclin-1 expression in patients with gastric cancer: a meta-analysis. Tumour Biol 2013 Aug 14; doi:10.1007/s13277-013-1049-8
He C, Levine B . The Beclin 1 interactome. Curr Opin Cell Biol 2010; 22:140–149.
Ciechomska IA, Goemans GC, Skepper JN, Tolkovsky AM . Bcl-2 complexed with Beclin-1 maintains full anti-apoptotic function. Oncogene 2009; 28:2128–2141.
Kang R, Zeh HJ, Lotze MT, Tang D . The Beclin 1 network regulates autophagy and apoptosis. Cell Death Differ 2011; 18:571–580.
Thoresen SB, Pedersen NM, Liestøl K, Stenmark H . A phosphatidylinositol 3-kinase class III sub-complex containing VPS15, VPS34, Beclin 1, UVRAG and BIF-1 regulates cytokinesis and degradative endocytic traffic. Exp Cell Res 2010; 316:3368–3378.
Ruck A, Attonito J, Garces KT, et al. The Atg6/Vps30/Beclin 1 ortholog BEC-1 mediates endocytic retrograde transport in addition to autophagy in C. elegans. Autophagy 2011; 7:386–400.
Gentile M, Ahnström M, Schön F, Wingren S . Candidate tumour suppressor genes at 11q23-q24 in breast cancer: evidence of alterations in PIG8, a gene involved in p53-induced apoptosis. Oncogene 2001; 20:7753–7760.
Zhao X, Ayer RE, Davis SL, et al. Apoptosis factor EI24/PIG8 is a novel endoplasmic reticulum-localized Bcl-2-binding protein which is associated with suppression of breast cancer invasiveness. Cancer Res 2005; 65:2125–2129.
Kim MS, Song SY, Lee JY, Yoo NJ, Lee SH . Expressional and mutational analyses of ATG5 gene in prostate cancers. APMIS 2011; 119:802–807.
Liu H, He Z, von Rütte T, et al. Down-regulation of autophagy-related protein 5 (ATG5) contributes to the pathogenesis of early-stage cutaneous melanoma. Sci Transl Med 2013; 5:202ra123.
Liang C, Feng P, Ku B, et al. Autophagic and tumour suppressor activity of a novel Beclin1-binding protein UVRAG. Nat Cell Biol 2006; 8:688–698.
Cheng Y, Ren X, Hait WN, Yang JM . Therapeutic targeting of autophagy in disease: biology and pharmacology. Pharmacol Rev 2013; 65:1162–1197.
Hampe J, Franke A, Rosenstiel P, et al. A genome-wide association scan of nonsynonymous SNPs identifies a susceptibility variant for Crohn disease in ATG16L1. Nat Genet 2007; 39:207–211.
Rioux JD, Xavier RJ, Taylor KD, et al. Genome-wide association study identifies new susceptibility loci for Crohn disease and implicates autophagy in disease pathogenesis. Nat Genet 2007; 39:596–604.
Baumgart DC, Sandborn WJ . Crohn's disease. Lancet 2012; 380:1590–1605.
Mizushima N, Noda T, Ohsumi Y . Apg16p is required for the function of the Apg12p-Apg5p conjugate in the yeast autophagy pathway. EMBO J 1999; 18:3888–3896.
Fujioka Y, Noda NN, Nakatogawa H, Ohsumi Y, Inagaki F . Dimeric coiled-coil structure of saccharomyces cerevisiae Atg16 and its functional significance in autophagy. J Biol Chem 2010; 285:1508–1515.
Gammoh N, Florey O, Overholtzer M, Jiang X . Interaction between FIP200 and ATG16L1 distinguishes ULK1 complex-dependent and -independent autophagy. Nat Struct Mol Biol 2013; 20:144–149.
Nishimura T, Kaizuka T, Cadwell K, et al. FIP200 regulates targeting of Atg16L1 to the isolation membrane. EMBO Rep 2013; 14:284–291.
Fujita N, Saitoh T, Kageyama S, Akira S, Noda T, Yoshimori T . Differential involvement of Atg16L1 in Crohn disease and canonical autophagy: analysis of the organization of the Atg16L1 complex in fibroblasts. J Biol Chem 2009; 284:32602–32609.
Saitoh T, Fujita N, Jang MH, et al. Loss of the autophagy protein Atg16L1 enhances endotoxin-induced IL-1β production. Nature 2008; 456:264–268.
Cadwell K, Liu JY, Brown SL, et al. A key role for autophagy and the autophagy gene Atg16l1 in mouse and human intestinal Paneth cells. Nature 2008; 456:259–263.
Marchiando AM, Ramanan D, Ding Y, et al. A deficiency in the autophagy gene Atg16L1 enhances resistance to enteric bacterial infection. Cell Host Microbe 2013; 14:216–224.
Parkes M, Barrett JC, Prescott NJ, et al. Sequence variants in the autophagy gene IRGM and multiple other replicating loci contribute to Crohn's disease susceptibility. Nat Genet 2007; 39:830–832.
McCarroll SA, Huett A, Kuballa P, et al. Deletion polymorphism upstream of IRGM associated with altered IRGM expression and Crohn's disease. Nat Genet 2008; 40:1107–1112.
Brest P, Lapaquette P, Souidi M, et al. A synonymous variant in IRGM alters a binding site for miR-196 and causes deregulation of IRGM-dependent xenophagy in Crohn's disease. Nat Genet 2011; 43:242–245.
Hampe J, Cuthbert A, Croucher PJ, et al. Association between insertion mutation in NOD2 gene and Crohn's disease in German and British populations. Lancet 2001; 357:1925–1928.
Hugot JP, Chamaillard M, Zouali H, et al. Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn's disease. Nature 2001; 411:599–603.
Ogura Y, Bonen DK, Inohara N, et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease. Nature 2001; 411:603–606.
Stappenbeck TS, Rioux JD, Mizoguchi A, et al. Crohn disease: a current perspective on genetics, autophagy and immunity. Autophagy 2011; 7:355–374.
Rubinsztein DC, Codogno P, Levine B . Autophagy modulation as a potential therapeutic target for diverse diseases. Nat Rev Drug Discov 2012; 11:709–730.
Ravikumar B, Vacher C, Berger Z, et al. Inhibition of mTOR induces autophagy and reduces toxicity of polyglutamine expansions in fly and mouse models of Huntington disease. Nat Genet 2004; 36:585–595.
Martinet W, Verheye S, De Meyer GR . Everolimus-induced mTOR inhibition selectively depletes macrophages in atherosclerotic plaques by autophagy. Autophagy 2007; 3:241–244.
Lin CI, Whang EE, Donner DB, et al. Autophagy induction with RAD001 enhances chemosensitivity and radiosensitivity through Met inhibition in papillary thyroid cancer. Mol Cancer Res 2010; 8:1217–1226.
Mita M, Sankhala K, Abdel-Karim I, Mita A, Giles F . Deforolimus (AP23573) a novel mTOR inhibitor in clinical development. Expert Opin Investig Drugs 2008; 17:1947–1954.
Thoreen CC, Kang SA, Chang JW, et al. An ATP-competitive mammalian target of rapamycin inhibitor reveals rapamycin-resistant functions of mTORC1. J Biol Chem 2009; 284:8023–8032.
Feldman ME, Apsel B, Uotila A, et al. Active-site inhibitors of mTOR target rapamycin-resistant outputs of mTORC1 and mTORC2. PLoS Biol 2009; 7:e38.
Sarkar S, Davies JE, Huang Z, Tunnacliffe A, Rubinsztein DC . Trehalose, a novel mTOR-independent autophagy enhancer, accelerates the clearance of mutant huntingtin and α-synuclein. J Biol Chem 2007; 282:5641–5652.
LaRocca TJ, Henson GD, Thorburn A, et al. Translational evidence that impaired autophagy contributes to arterial ageing. J Physiol 2012; 590:3305–3316.
Hidvegi T, Ewing M, Hale P, et al. An autophagy-enhancing drug promotes degradation of mutant α1-antitrypsin and reduces hepatic fibrosis. Science 2010; 329:229–232.
Shoji-Kawata S, Sumpter R, Leveno M, et al. Identification of a candidate therapeutic autophagy-inducing peptide. Nature 2013; 494:201–206.
Fedorko M . Effect of chloroquine on morphology of cytoplasmic granules in maturing human leukocytes—an ultrastructural study. J Clin Invest 1967; 46:1932–1942.
Amaravadi RK, Yu D, Lum JJ, et al. Autophagy inhibition enhances therapy-induced apoptosis in a Myc-induced model of lymphoma. J Clin Invest 2007; 117:326–336.
Amaravadi RK, Lippincott-Schwartz J, Yin XM, et al. Principles and current strategies for targeting autophagy for cancer treatment. Clin Cancer Res 2011; 17:654–666.
McAfee Q, Zhang Z, Samanta A, et al. Autophagy inhibitor Lys05 has single-agent antitumor activity and reproduces the phenotype of a genetic autophagy deficiency. Proc Natl Acad Sci USA 2012; 109:8253–8258.
Seglen PO, Gordon PB . 3-Methyladenine: specific inhibitor of autophagic/lysosomal protein degradation in isolated rat hepatocytes. Proc Natl Acad Sci USA 1982; 79:1889–1892.
Wu Y, Wang X, Guo H, et al. Synthesis and screening of 3-MA derivatives for autophagy inhibitors. Autophagy 2013; 9:595–603.
Miller S, Tavshanjian B, Oleksy A, et al. Shaping development of autophagy inhibitors with the structure of the lipid kinase Vps34. Science 2010; 327:1638–1642.
Sugawara K, Suzuki NN, Fujioka Y, et al. Structural basis for the specificity and catalysis of human Atg4B responsible for mammalian autophagy. J Biol Chem 2005; 280:40058–40065.
Kumanomidou T, Mizushima T, Komatsu M, et al. The crystal structure of human Atg4b, a processing and de-conjugating enzyme for autophagosome-forming modifiers. J Mol Biol 2006; 355:612–618.
Noda N, Satoo K, Fujioka Y, et al. Structural basis of Atg8 activation by a homodimeric E1, Atg7. Mol Cell 2011; 44:462–475.
Taherbhoy A, Tait S, Kaiser S, et al. Atg8 transfer from Atg7 to Atg3: a distinctive E1-E2 architecture and mechanism in the autophagy pathway. Mol Cell 2011; 44:451–461.
Mizushima N, Yoshimori T, Levine B . Methods in mammalian autophagy research. Cell 2010; 140:313–326.
Kuma A, Matsui M, Mizushima N . LC3, an autophagosome marker, can be incorporated into protein aggregates independent of autophagy: caution in the interpretation of LC3 localization. Autophagy 2007; 3:323–328.
Martin LJ, Gupta J, Jyothula SS, et al. Functional variant in the autophagy-related 5 gene promotor is associated with childhood asthma. PLoS One 2012; 7:e33454.
Poon A, Eidelman D, Laprise C, Hamid Q . ATG5, autophagy and lung function in asthma. Autophagy 2012; 8:694–695.
Zhou XJ, Lu XL, Lv JC, et al. Genetic association of PRDM1-ATG5 intergenic region and autophagy with systemic lupus erythematosus in a Chinese population. Ann Rheum Dis 2011; 70:1330–1337.
Pierdominici M, Vomero M, Barbati C, et al. Role of autophagy in immunity and autoimmunity, with a special focus on systemic lupus erythematosus. FASEB J 2012; 26:1400–1412.
Barrett JC, Hansoul S, Nicolae DL, et al. Genome-wide association defines more than 30 distinct susceptibility loci for Crohn's disease. Nat Genet 2008; 40:955–962.
Zhao YG, Zhao H, Miao L, et al. The p53-induced gene Ei24 is an essential component of the basal autophagy pathway. J Biol Chem 2012; 287:42053–42063.
Franke A, Balschun T, Sina C, et al. Genome-wide association study for ulcerative colitis identifies risk loci at 7q22 and 22q13 (IL17REL). Nat Genet 2010; 42:292–294.
Laurin N, Brown JP, Morissette J, et al. Recurrent mutation of the gene encoding sequestosome 1 (SQSTM1/p62) in Paget disease of bone. The Am J Hum Genet 2002; 70:1582–1588.
Rubino E, Rainero I, Chiò A, et al. SQSTM1 mutations in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Neurology 2012; 79:1556–1562.
Hirano M, Nakamura Y, Saigoh K, et al. Mutations in the gene encoding p62 in Japanese patients with amyotrophic lateral sclerosis. Neurology 2013; 80:458–463.
Martinez-Outschoorn UE, Pavlides S, Whitaker-Menezes D, et al. Tumor cells induce the cancer associated fibroblast phenotype via caveolin-1 degradation: implications for breast cancer and DCIS therapy with autophagy inhibitors. Cell Cycle 2010; 9:2423–2433.
Rojas-Puentes L, Gonzalez-Pinedo M, Crismatt A, et al. Phase II randomized, double-blind, placebo-controlled study of whole-brain irradiation with concomitant chloroquine for brain metastases. Radiat Oncol 2013; 8:209.
Fornai F, Longone P, Cafaro L, et al. Lithium delays progression of amyotrophic lateral sclerosis. Proc Natl Acad Sci USA 2008; 105:2052–2057.
Acknowledgements
This work was supported by the Funding Program for Next Generation World-Leading Researchers, and JSPS KAKENHI Grants-in-Aid for Scientific Research on Innovative Areas (25111005) (to NM). PJ is supported by a scholarship from the China Scholarship Council in China and by the Ministry of Education, Culture, Sports, Science, and Technology in Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jiang, P., Mizushima, N. Autophagy and human diseases. Cell Res 24, 69–79 (2014). https://doi.org/10.1038/cr.2013.161
Published:
Issue Date:
DOI: https://doi.org/10.1038/cr.2013.161
Keywords
This article is cited by
-
Ratiometric and discriminative visualization of autophagic processes with a novel dual-responded lysosome-specific fluorescent probe
Biomaterials Research (2023)
-
The Role of Decreased Levels of Neuronal Autophagy in Increased Susceptibility to Post-traumatic Epilepsy
Neurochemical Research (2023)
-
Biogenic Selenium Nanoparticles Synthesized by Lactobacillus casei ATCC 393 Alleviate Acute Hypobaric Hypoxia-Induced Intestinal Barrier Dysfunction in C57BL/6 Mice
Biological Trace Element Research (2023)
-
In Silico Study of ULK1 Gene as a Susceptible Biomarker for Neurodegeneration
Proceedings of the National Academy of Sciences, India Section B: Biological Sciences (2023)
-
Quercetin potentiates the anti-osteoporotic effects of alendronate through modulation of autophagy and apoptosis mechanisms in ovariectomy-induced bone loss rat model
Molecular Biology Reports (2023)