Abstract
Objective: To compare the rate and extent of absorption of DL-threo-methylphenidate (MPH) from two modified-release MPH formulations at their respective recommended starting doses in healthy adult volunteers.
Design: Open-label, randomised, crossover, bioavailability study.
Participants: Twenty healthy adult male and female volunteers.
Methods: Subjects received single doses of two modified-release formulations of MPH, a 20mg capsule (Ritalin® LA) and an 18mg tablet (Concerta®). A total of 19 plasma samples was collected over 24 hours, and MPH plasma concentrations were determined by liquid chromatography-mass spectrometry (LC-MS/MS). These values were used to calculate standard noncompartmental pharmacokinetic parameters describing the rate (peak concentration and time to peak concentration) and extent (area under the concentration-time curve, AUC) of absorption of the two formulations. The relative bioavailability of the two drugs was assessed using a 90% confidence interval, based on the lower and upper endpoints of the confidence interval for the ratios of the geometric means (log transformed) being within the 0.80–1.25 equivalence criterion.
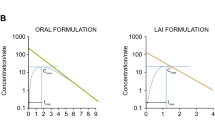
Results: Nineteen subjects, ten male and nine female, aged 21–34 years completed both treatment phases of the study. The Ritalin® LA formulation displayed a distinctly biphasic pharmacokinetic profile, with mean initial peak plasma concentration of 7 µg/L at an average of 2.1 hours after administration and a second peak of 9.3 µg/L occurring at 5.6 hours. In contrast, the profile of the Concerta® formulation rapidly reached an initial plateau concentration of 3.4 µg/L at 3.3 hours after administration and a second mean plateau concentration of 5.9 µg/L approximately 6 hours after administration. Substantially more MPH was absorbed from Ritalin® LA than from Concerta® over the first 4 hours; the respective AUC4 values were 18.5 and 9.3 µg · h/L (p < 0.001). The overall extent of absorption of MPH was similar between the two formulations. Oral clearance was identical between the two dosage forms.
Conclusion: The Ritalin® LA formulation exhibited more rapid initial absorption and reached significantly higher peak plasma concentrations compared with the Concerta® formulation, although the oral bioavailability of MPH was similar between the two formulations. The Ritalin® LA capsule demonstrated a distinctly bimodal plasma concentration-time profile. MPH plasma concentrations resulting from Concerta® reached a peak at 6 hours. These results indicate that the recommended starting dose of the Ritalin® LA 20mg capsule formulation provides more rapid absorption and higher peak plasma concentrations than the recommended 18mg starting dose of the Concerta® formulation.




Similar content being viewed by others
Notes
Use of tradenames is for product identification only and does not imply endorsement.
References
Cantwell DP. Attention deficit disorder: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry 1996; 35: 978–87
Dulcan M, Work Group on Quality Issues. Practice parameters for the assessment and treatment of children, adolescents, and adults with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 1997; 36: 85S–121S
Swanson JM, Seargent JA, Taylor E, et al. Attention deficit disorder and hyperkinetic disorder. Lancet 1998; 351: 429–33
Mannuzza S, Klein RG, Bessler A, et al. Adult psychiatric status of hyperactive boys grown up. Am J Psychiatry 1998; 155: 493–8
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, fourth edition, text revision. Washington, DC: American Psychiatric Association, 2000
Tannock R. Attention deficit hyperactivity disorder: advances in cognitive, neurobiological, and genetic research. J Child Psychol Psychiatry 1998; 39: 65–99
Spencer T, Biederman J, Wilens T. Attention-deficit/hyperactivity disorder and comorbidity. Pediatr Clin North Am 1999; 46: 915–27
Faraone SV, Biederman J. Neurobiology of attention-deficit hyperactivity disorder. Biol Psychiatry 1998; 44: 951–8
Patrick KS, Markowitz JS. Pharmacology of methylphenidate, amphetamine enantiomers and pemoline in attention-deficit hyperactivity disorder: a review. Hum Psychopharmacol 1997; 12: 527–46
Kratochvil CJ, Heiligenstein JH, Dittmann R, et al. Atomoxetine and methylphenidate treatment in children with ADHD: a prospective, randomized, open-label trial. J Am Acad Child Adolesc Psychiatry 2002; 41: 776–84
Elia J, Ambrosini PJ, Rapoport JL. Treatment of attention-deficit-hyperactivity disorder. N Engl J Med 1999; 340: 780–8
Goldman LS, Genel M, Bezman RJ, et al. Diagnosis and treatment of attention-deficit/hyperactivity disorder in children and adolescents. JAMA 1998; 279: 1100–7
American Academy of Pediatrics, Subcommittee on Attention-Deficit/Hyperactivity Disorder, Committee on Quality Improvement. Clinical practice guideline: treatment of the school-aged child with attention-deficit/hyperactivity disorder. Pediatrics 2001; 108: 1033–44
Pliszka SR, Greenhill LL, Crismon ML, et al. The Texas children’s medication algorithm project: report of the Texas consensus conference panel on medication treatment of childhood attention-deficit/hyperactivity disorder: Part I. attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 2000; 39: 908–19
NIH Consensus Statement Online. Diagnosis and treatment of attention deficit hyperactivity disorder. Available from URL: http://odp.od.nih.gov/consensus/cons/110/110_statement.htm. [Accessed 2002 Jun 14]
Greenhill LL, Pliszka S, Dulcan MK, et al. Practice parameters for the use of stimulant medications in the treatment of children, adolescents, and adults. J Am Acad Child Adolesc Psychiatry 2002; 41 (2 Suppl.): 26S–49S
Wargin W, Patrick K, Kilts C, et al. Pharmacokinetics of methylphenidate in man, rat and monkey. J Pharmacol Exp Ther 1983; 226: 382–6
Meyer MC, Straughn AB, Jarvi EJ, et al. Bioequivalence of methylphenidate immediate-release tablets using a replicated study design to characterize intrasubject variability. Pharm Res 2000; 17: 381–4
Patrick KS, Straughn AB, Jarvi EJ, et al. The absorption of sustained-release methylphenidate formulation compared to an immediate-release formulation. Biopharm Drug Dispos 1989; 10: 165–71
Swanson JM, Volkow ND. Pharmacokinetic and pharmacodynamic properties of stimulants: implications for the design of new treatments for ADHD. Behav Brain Res 2002; 130: 73–8
Swanson J, Gupta S, Guinta D, et al. Acute tolerance to methylphenidate in the treatment of attention deficit hyperactivity disorder in children. Clin Pharmacol Ther 1999; 66: 295–305
Swanson J, Kinsbourne M, Roberts W, et al. Time-response analysis of the effect of stimulant medication on the learning ability of children referred for hyperactivity. Pediatrics 1978; 61: 21–7
Perel JM, Greenhill LL, Curran S, et al. Correlates of pharmacokinetics and attentional measures in methylphenidate treated hyperactive children. Clin Pharmacol Ther 1991; 49: 160–1
Greenhill LL. Pharmacologic treatment of attention deficit hyperactivity disorder. Psychiatr Clin North Am 1992; 15: 1–27
Modi NB, Lindemulder B, Gupta SK. Single- and multipledose pharmacokinetics of an oral once-a-day osmotic controlled-release OROS® (methylphenidate HCl) formulation. J Clin Pharmacol 2000; 40: 379–88
Modi NB, Wang B, Hu WT, et al. Effect of food on the pharmacokinetics of osmotic controlled-release methylphenidate HCl in healthy subjects. Biopharm Drug Dispos 2000; 21: 23–31
Modi NB, Wang B, Noveck RJ, et al. Dose-proportional and stereospecific pharmacokinetics of methylphenidate delivered using an osmotic, controlled-release oral delivery system. J Clin Pharmacol 2000; 40: 1141–9
Anonymous. Concerta® prescribing information. Mountain View, CA: ALZA Corporation, 2000
Keating GM, Figgitt DP. Dexmethylphenidate. Drugs 2002; 62: 1899–904
Swanson J, Greenhill, Pelham W, et al. Initiating Concerta™ (OROS® methylphenidate HCl) qd in children with attentiondeficit hyperactivity disorder. J Clin Res 2000; 3: 59–76
Gualtieri CT, Wargin W, Kanoy R, et al. The effect of eating and fasting on the absorption of methylphenidate. Res Commun Psychol Psychiatr Behav 1982; 7: 381–4
Chan YM, Swanson JM, Solin SS, et al. Methylphenidate hydrochloride given with or before breakfast: II. effects on plasma concentration of methylphenidate and ritalinic acid. Pediatrics 1983; 72: 56–9
Midha KK, McKay G, Rawson MJ, et al. Effects of food on pharmacokinetics of methylphenidate. Pharm Res 2001; 18: 1185–9
Lee L, Kepple J, Wang Y, et al. Bioavailability of modified-release methylphenidate: influence of high-fat breakfast when administered intake and when capsule content sprinkled on applesauce. Biopharm Drug Dispos. In press
Gonzalez MA, Pentkis HS, Anderi N, et al. Methylphenidate bioavailability from two extended-release formulations. Int J Clin Pharmacol Ther 2002; 40: 175–84
Gualteri CT, Hicks RE, Patrick K, et al. Clinical correlates of methylphenidate blood levels. Ther Drug Monit 1984; 6: 379–92
Acknowledgments
This study was supported by Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA. The authors would like to acknowledge Dr Bernd Meibohm and Dr Ryan Yates for their assistance in the conduct of the clinical protocol. The authors further acknowledge the analytical assay development and support of Dr Fred Brill of National Medical Services, Willow Grove, PA, USA. The authors have provided no information on conflicts of interest directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Markowitz, J.S., Straughn, A.B., Patrick, K.S. et al. Pharmacokinetics of Methylphenidate After Oral Administration of Two Modified-Release Formulations in Healthy Adults. Clin Pharmacokinet 42, 393–401 (2003). https://doi.org/10.2165/00003088-200342040-00007
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-200342040-00007